While you can rely on Taylor Swift and Adele to help heal emotional heartbreak, unfortunately treating a physically “broken” heart, a heart damaged by fibrosis, is a much more complicated process than putting on your favorite sad songs and wallowing in your feelings. In a recent study published in Science, researchers developed a therapeutic approach to treat damaged hearts in mice through the removal of scar tissue using genetically engineered immune cells (CAR T cells) and the mRNA technology used in the mRNA coronavirus vaccines.

Don’t Go Breaking My Heart
Cardiac fibrosis, the stiffening and scarring of heart tissue, affects millions of people worldwide suffering from cardiovascular diseases. Though the human body is remarkably adept at healing itself in many ways, and capable of rebuilding after enduring disease and injury, not all injuries can be easily overcome or regenerated, especially when it comes to the heart.
When myocardial injury occurs, cardiac fibroblasts, cells that produce connective tissue in the heart, are activated and function as the principle cells responsible for “remodeling” the damage by secreting extracellular matrix (ECM). This can initially be a beneficial and protective mechanism that assists with tissue regeneration and wound healing when the damage is minor and non-repetitive. However, in many chronic cardiovascular diseases, myocardial damage is repetitive and can be severe. As a result fibroblasts continue to secrete excessive ECM, leading to fibrosis and impaired heart function.
Thus far, clinical trials for antifibrotic therapeutics have demonstrated only a modest effect at best, and are designed only to limit fibrotic progression, not remodel or repair the fibrotic damage. Given the significant impact of cardiac fibrosis and overall worldwide burden of heart disease as the leading cause of death globally, the research team wanted to develop a therapeutic approach that could both reduce fibrosis and restore cardiac function.
How Can You Mend A Broken Heart?
In this study, researchers designed their therapeutic approach to leverage and combine two key technologies: genetically engineered T cells and mRNA lipid nanoparticles.
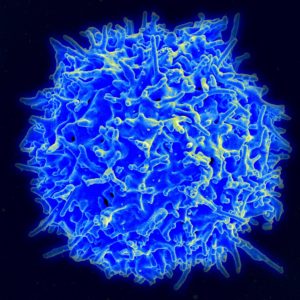
T cells are immune cells that play a critical role in the body’s immunity to foreign substances. These cells use receptors on their surface to recognize antigens that are specific to a number of foreign particles, from viruses to allergens to tumors. The T cell binds to those antigens and help trigger other parts of the immune system to respond and destroy the intruder.
Chimeric antigen receptor T cells (CAR T cells) are T cells that have been genetically engineered by adding in a gene for a synthetic man-made receptor protein, known as a chimeric antigen receptor or CAR, which allows the cells to be “reprogrammed” to identify the desired specific antigen and initiate targeted immune responses to said antigen.
CAR T cell therapy is already being used as a type of personalized cancer treatment that can be very effective, particularly in treating cancers of the blood such as leukemia. However, these treatments are extremely time-consuming and expensive. The process of making conventional CAR T cells involves collecting the patient’s T cells through leukapheresis, sending them to the lab to be genetically engineered, grown and multiplied (which can take several weeks), and returned to the patient in the form of an infusion.
Keeping this in mind, the approach of this study was to avoid the removal of T cells from the patient altogether, which could be accomplished by packing modified messenger RNA (mRNA) into lipid nanoparticles (LNPs) that are capable of producing CAR T cells in vivo after injection. This LNP-mRNA technology was foundational to the development, success and safety of the mRNA COVID-19 vaccines, and has driven efforts to extend and apply this therapeutic platform to additional pathologies.
The researchers generated a modified mRNA encoding for a CAR designed against FAP (fibroblast activation protein), which is a marker of activated fibroblasts, and then packaged it inside CD5-targeting LNPs. CD5 is a glycoprotein receptor that is naturally expressed on the surface of all T cells. They were then able to evaluate the efficacy of these modified mRNA-LNPs by injecting them into a mouse model of heart failure.
My Heart Will Go On
The team observed efficient delivery of the modified mRNA encoding CAR to T cells. This accomplished the goal of producing effective, transient CAR T cells in vivo and offers proof of concept that modified mRNA encapsulated in targeted LNPs can be delivered intravenously as a means of producing functional engineered T cells entirely inside the body.
Two weeks following the infusion of modified mRNA-targeted LNPs, analysis of the mouse model revealed that the treatment was successful in reducing fibrosis and restoring cardiac function after injury. The amount of scar tissue in the hearts of the mice was nearly halved in comparison to the untreated mice and the heart function of the treated mice also improved significantly.
This modified mRNA-targeted LNP approach could be a promising therapeutic method with far-reaching potential applications. As a therapeutic method, it could dramatically decrease costs and is also transient by design, given that mRNA is intrinsically unstable, restricted to the cytoplasm and thus incapable of integrating into (and permanently altering) the genome, and is diluted during cell division. This transient nature makes it a particularly attractive method for treatment of certain disorders as it is likely to help limit toxicities and offer the advantageous ability to titrate dosing. In vivo generation of CAR T cells may also be a promising approach for treating fibrosis of other organs, such as the liver, intestines and kidney.
References:
- Rurik, J.G. et al. (2021) CAR T cells produced in vivo to treat cardiac injury. Science. 375(6576), 23–24.
- Hinderer, S. and Schenke-Layland, K. (2019) Cardiac fibrosis – A short review of causes and therapeutic strategies. Advanced Drug Delivery Reviews. 146, 77–82.
- Henderson, N.C., Rieder, F., and Wynn, T.A. (2020) Fibrosis: from mechanisms to medicines. Nature. 587, 555–566.
- CAR T-cell Therapy and Its Side Effects. Cancer.org. Accessed January 2022.
- mRNA vaccine technology has helped repair broken hearts in mice. NewScientist. Accessed January 2022.
This study used our Luciferase Assay System which have a wide range of applications. Learn more about our luciferase assays here.
Want to read more about this technology? These blogs about luciferase reporter assays are a great place to start.
