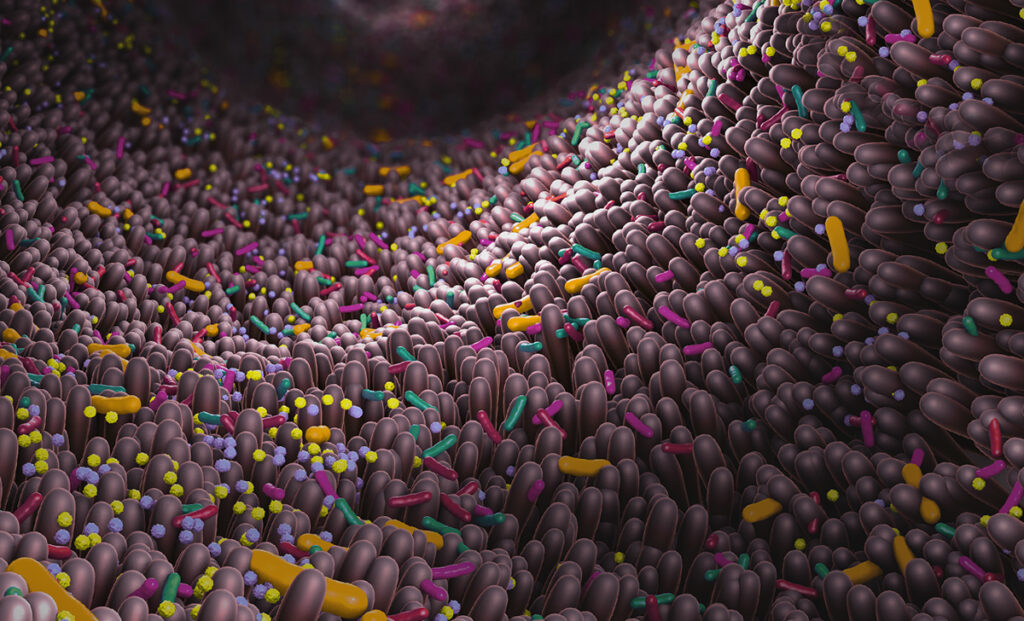
The human microbiome, the bustling cooperative of all the microscopic creatures that naturally colonize in and on our bodies, wields a surprising amount of influence over many of the unseen processes that are critical to our overall health and wellness. Over the course of decades, we have learned that this is particularly true for the microbes that reside in our gastrointestinal tract, collectively known as our gut microbiota.
Our gut microbiota is constantly communicating with our bodies, though our relationship with our gut can feel like trying to have a conversation with someone who only speaks a language we do not know or understand—you can take an educated guess at what they are saying based on their expressions and gestures, but the true message and meaning behind their actions is not always discernable. So while we can feel that someone in our gut is unhappy when we have a tummy ache, the true mechanism behind exactly who is unhappy and why, is not as obviously deduced or understood.
What if there was a tool that could help us more easily interpret the language of our microbiota, giving us the means to both better understand our microbiomes as well as to detect biomarkers of various diseases? Recent studies have shown that such a solution may be (quite literally) right under our noses: our breath.
Gut Feelings
The gut microbiota is one of the most complex and densely populated microbial ecosystems, not only in the human body, but also the world, containing a number of archaea, fungi, protist and viral species, in addition to 300 to 500 bacterial species. Over time, the dynamics of our host relationship to our gut microbiota have evolved to form a powerful symbiosis, in which we provide the environment these microbes need to thrive in exchange for the fulfillment of a number of essential functions that help absorb nutrients, maintain homeostasis, and protect us from pathogens. Despite the many benefits, however, the intrinsic entwining of our bodies with our microbial counterparts can negatively impact our health when an imbalance occurs in the gut microbiota.
There is a growing evidence base indicating strong links between dysregulation of the human gut microbiota and a number of autoimmune and inflammatory health conditions. For some of these conditions, it can be easier to trace the connection between an imbalanced gut microbiome and the resulting ailment, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and systemic manifestations of diseases like obesity and Type 2 diabetes. However, many studies have reported changes in the gut microbiota as a contributor to a number of conditions where such a connection is not as obvious, including liver diseases like non-alcoholic steatohepatitis, cardiometabolic diseases and disorders, neurodegenerative diseases such as Alzheimer’s, Parkinson’s, multiple sclerosis and Huntington’s disease, and both direct and indirect contributions to cancerous tumor initiation and progression.
In addition to the pathophysiological role it plays in the development of so many illnesses and disorders, the gut microbiome can also impact the pharmacokinetics of drugs, adding another layer of complication to disease treatment, progression and management. This ability of the gut microbiota to influence the metabolism of therapeutic drugs (e.g., the presence of a particular bacterium could metabolize an active pharmaceutical ingredient of a drug, producing an inactive metabolite in its place) emphasizes the importance of a personalized approach to medicine, as each person’s microbiome can differ in composition and thus differ in the way we each respond to pharmaceutical interventions.
A Breath of Fresh Volatile Air
Due to the considerable evidence base linking our gut microbiota to a number of diseases and the understanding that our health relies considerably upon the the many metabolites produced by our gut flora, it’s becoming increasingly evident that a simple solution to easily identify and interpret the activity of species in our microbiota is needed—and some of these metabolites may hold the key.
One type of metabolite our gut microbiota produce are gaseous carbon-based molecules known as volatile organic compounds, or VOCs. VOC metabolites released in the gut, typically produced as waste products from the metabolism and fermentation of food, first get absorbed into the bloodstream, then distributed throughout the many tissues and organs in our bodies, and finally make their way up to our lungs where they are ultimately expelled through exhaled breath.
With many of the diseases that are linked to dysregulation of the gut microbiota, deviation of various metabolic pathways occurs, leading to altered concentrations of different VOCs which can be observed in a number of avenues in the body, including cell lines, tissues, bodily fluids and exhaled breath. Recent studies have been exploring using VOCs detected in exhaled breath as biomarkers investigate activities of the gut microbiota.
The idea of measuring gases via breath test is not a brand new concept. One existing diagnostic application are hydrogen and methane breath test (HMBT) kits, which measure the hydrogen and methane produced in the gut microbiome and the specific concentrations of which can be used to diagnose conditions like SIBO (small intestine bacterial overgrowth) and carbohydrate malabsorption which can include conditions like lactose intolerance. Considering the number of conditions associated with our gut microbiota that have the ability to impact VOC concentrations, it’s clear that breath sampling is an untapped and promising avenue to further detect and elucidate a number of microbial biomarkers.
Catching Your Breath
Currently, the methodologies used to evaluate how the gut microbiome impacts human health are centered around the microbial metabolites they produce, all of which are typically analyzed by way of blood, urine or fecal samples. The option to employ breath tests to study volatile microbial metabolites in exhaled breath offers a more user-friendly, standardized methodology with numerous benefits.
First of all, due to its continuous and renewable nature, breath is an essentially limitless resource. This method allows samples to be preconcentrated, enhancing the sensitivity of the analysis. Breath tests are also intrinsically non-invasive, making them particularly appealing option to patients, clinicians, and clinical researchers alike. This stands in stark contrast to the invasive biopsy procedures typically associated with disease monitoring and diagnosis, which also pose additional patient risks like infection and tissue damage. Beyond just the safety advantages of invasive procedures, breath tests also circumvent the expense that accompanies such procedures, offering a much more cost-effective alternative.
The non-invasive nature of breath sampling is additional advantageous in that it allows easy sample collection at regular intervals, enabling simple monitoring of various metabolic pathways. This aspect would be particularly beneficial in clinical trials, offering essentially real-time insights into participants’ responses to treatments and evaluation of potential markers for pharmacodynamics, pharmacokinetics, efficacy and safety—a frequency of information acquisition that would be extremely challenging to replicate using more invasive techniques. The potential of portability of breath tests is another major advantage, providing an option for collection that can take place anywhere, forgoing the need for frequent trips to the clinic.
Though researchers are only beginning to scratch the surface of this innovative approach, breath testing offers a promising approach for personalized, portable, non-invasive diagnostic and monitoring tools that have the potential to continue demystifying microbial biomarkers and the roles they play in disease pathophysiology and progression.
References
- Ball, M. and Boyle, B. (2023) Breath Can Deepen Our Understanding of the Microbiome. GEN: Genetic Engineering & Biotechnology News.
- Bhandari, M.P. et al. (2023) Volatile Markers for Cancer in Exhaled Breath—Could They Be the Signature of the Gut Microbiota? Molecules. 28(8), 3488.
- Breton, J. (2019) The Gut Microbiota: A Symbiotic Relationship with Humans. Microbiome Foundation. Accessed August 2023.
- Bull, M.J. and Plummer, N.T. (2014) Part 1: The Human Gut Microbiome in Health and Disease. Integr. Med (Encinitas). 13(6), 17–22.
- Lozupone, C.A. et al. (2012) Diversity, Stability and Resilience of the Human Gut Microbiota. Nature. 489(7415), 220–230.
- Quigley, E.M.M. (2013) Gut Bacteria in Health and Disease. Gastroenterol. Hepatol. (NY). 9(9), 560–569.
