RNA doesn’t just carry genetic instructions—it also interacts with proteins to regulate nearly every aspect of gene expression, from splicing to translation. When those interactions go awry, the consequences can be devastating. In myotonic dystrophy type 1 (DM1), the most common adult-onset muscular dystrophy, a toxic RNA repeat expansion hijacks a critical protein called MBNL1, trapping it in nuclear clumps called foci. This leads to widespread splicing defects and progressive muscle wasting. But studying these toxic interactions inside living cells—and finding small molecules that can disrupt them—has been a significant challenge.
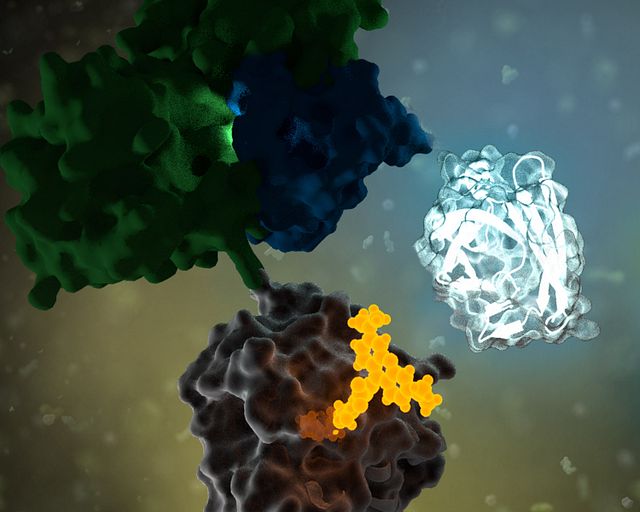
A recent study led by the Scripps Institute may have a solution. The study introduces a NanoBRET™ assay that can monitor the interaction between the expanded CUG RNA repeats and MBNL1 protein in real time, in live cells. Their findings demonstrate how this platform can be used not only to detect disease-driving RNA–protein complexes but also to identify small molecules that break them apart.
Continue reading “A Live-Cell NanoBRET Assay Shines Light on Toxic RNA–Protein Interactions in Myotonic Dystrophy”