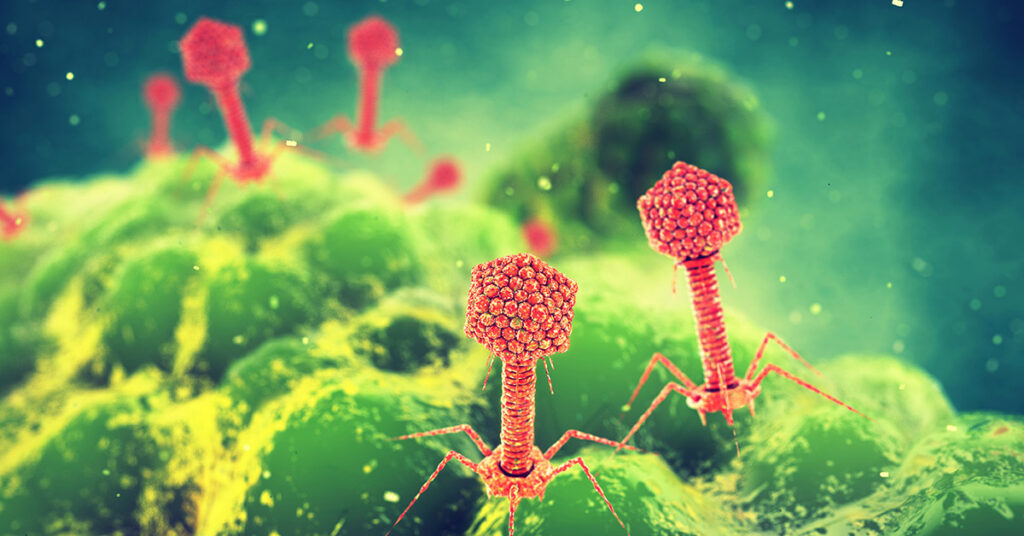
Global pandemics, such as COVID-19, have taught us to abhor viruses. The emergence of new, highly infectious viruses is—rightfully so—a cause for concern. However, despite the average human body harboring 380 trillion viruses, most of them simply coexist with us and are harmless. When it comes to an ancient lineage of viruses within the realm Duplodnaviria, researchers are even using them as weapons in the battle against infectious diseases.
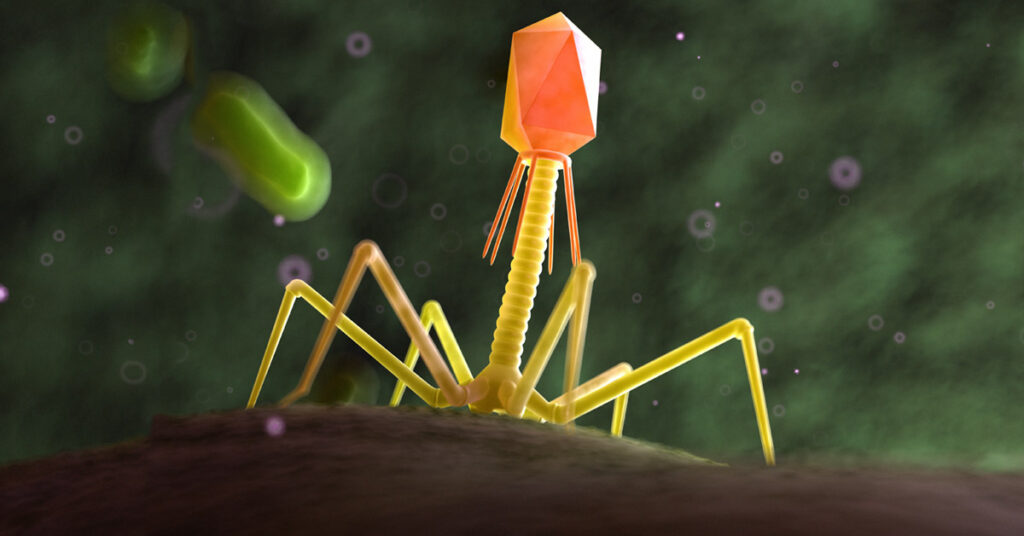
In 1915, Frederick William Twort, an English bacteriologist at the University of London, reported the discovery of an unusual “ultramicroscopic virus” (1). Twort was culturing vaccinia virus as part of an experiment to determine if he could prepare smallpox vaccines in vitro. These vaccines, made in calves, were typically contaminated with Staphylococcus bacteria. When Twort plated the vaccines, he found small, clear areas on the agar plates where the bacteria would not grow, and these clear areas were the source of his ultramicroscopic virus. Two years later, a French-Canadian microbiologist, Félix d’Hérelle, independently discovered a similar phenomenon when culturing Shigella bacteria from fecal samples of patients with bacillary dysentery. He called the new virus “un bactériophage obligatoire” (2). Shortly after his discovery, he found that bacteriophages (phages) could be used as powerful agents to treat a variety of bacterial infections, and the field of phage therapy was born (3).
This revolutionary approach was not without controversy (3). Although phage therapy was widely used up to and during World War II, the commercial production of antibiotics after the war led to decreased interest in phage therapy, especially in the US. In recent years, phage therapy is enjoying resurgent popularity, largely due to the emergence of antibiotic-resistant strains of bacteria.
When Antibiotics Fail, Phage Therapy Steps In
Sabrina Green, PhD, is a postdoctoral research associate at the Lab of Gene Technology, Katholieke Universiteit (KU) Leuven, Belgium. The university, founded in 1425, is home to one of the world’s leading research programs in bacteriophage therapy. Dr. Green’s PhD research focused on the pathogenesis of multidrug-resistant (MDR) extraintestinal pathogenic E. coli and developing model systems to study this pathogen. “Naturally, the next step was to develop an effective therapy or preventative for these infections,” she says, “which led me to phage therapy.”

The goal of Dr. Green’s project was to eradicate antibiotic-resistant E. coli from the gut, without harming beneficial E. coli strains that are an important part of the human microbiome. “Phages are perfect for this because they are highly specific,” Dr. Green says. “They can target bacteria in these complex communities, without causing major changes to the microbiota.” Her experiments demonstrated the effectiveness of phage therapy in eradicating pathogenic E. coli in animal models.
The next step was to translate these results into a clinical setting. Phage therapy trials around the world had shown promising results, and Dr. Green knew the treatment was safe and effective. “I wanted to give more people access to this treatment, so we developed a not-for-profit phage center in Houston, Texas to source and prepare phages for patients with difficult-to-treat infections.” Currently, in Belgium, she is working with researchers who have treated more than a hundred patients with phage therapy, and their results have proven the safety and effectiveness of this treatment.
Phage therapy offers an attractive alternative to conventional methods when patients develop infections from antibiotic-resistant bacteria. Dr. Green notes that these patients often have no viable treatment options. “They are in a never-ending cycle of getting antibiotic treatment, then returning later for treatment again,” she says. “Some are in constant pain due to infections, like chronic urinary tract infections. Some patients have to get surgery due to infections.” These treatments can put patients at risk for even more infections and, potentially, more dire situations. However, sometimes antibiotics and phage therapy can synergize, so antibiotics can potentially be included in treatments as well.
Can phage therapy cause significant changes to the normal human microbiome? Dr. Green observes that, in her experiments, she saw no significant changes to the microbiome, using the specific E. coli phages that she tested. She doesn’t rule out the potential for some changes to occur. However, she says, “When you compare it to significant changes that occur with antibiotic use, it is clear that phages are a better approach for targeted therapy.”
Beyond Natural Phages
How do we treat infectious diseases caused by MDR bacteria if there are no naturally occurring phages available to target the pathogenic bacteria? One approach that’s showing promise is the use of CRISPR-Cas9 gene editing technology to create modified bacteriophages. Eligo Bioscience (Paris, France) is one company using CRISPR-based targeting approaches to target pathogenic bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA) and pathogenic strains of Cutibacterium acnes (4). Other companies commercializing phage therapy include BiomX (Ness Ziona, Israel), Armata Pharmaceuticals (Los Angeles, California), Adaptive Phage Therapeutics (Gaithersburg, Maryland; recently acquired) and SNIPR Biome (Copenhagen, Denmark).
Another therapeutic option for drug-resistant bacterial infections involves endolysins, which are phage-encoded enzymes that lyse bacteria by specifically hydrolyzing the bacterial cell wall of Gram-positive bacteria. Endolysins have proved effective in combating several common Gram-positive pathogens, including MRSA, Bacillus anthracis, Streptococcus pneumoniae and Clostridium perfringens (reviewed in 5, 6).
For Gram-negative bacteria, a modified endolysin approach is necessary, due to their protective outer lipopolysaccharide layer. “You would have to engineer them to get through the outer membrane,” Dr. Green says. “Some work by Rob Lavigne, Yves Briers and others have shown this to be an effective approach.” (7)
Now, Next, Later
Dr. Green’s current research project involves sequencing and analyzing genomes from bacterial samples from patients that have received phage therapy in Belgium. She is also developing phage therapy for a more complex inflammatory disease called hidradenitis suppurativa, in which patients develop painful lumps deep in the skin. “Patients with this disease get very painful lesions and are on constant antibiotic treatment,” Dr. Green says. A review of this research is now available as a preprint (8).
What does the future hold for phage therapy? “When I think of the future,” Dr. Green says, “I think of this paper I read by Jean-Paul Pirnay called ‘Phage therapy in the year 2035.’” (9) The author envisions a future in which a device is invented that can make and purify phage on the spot, using artificial intelligence (AI) to generate the correct phage targeted specifically at the bacteria causing the disease. Dr. Green concludes, “The challenges that we have today will be solved when we invest in future technology that can advance the field of phage therapy.”
Interested in learning more about basic life science research? Check out Promega Notes for feature stories, research highlights and technical tips.
References
- Twort, F.W. (1915) An investigation on the nature of ultra-microscopic viruses. Lancet 186(4814), 1241–1243.
- d’Hérelle, F. (1917) On an invisible microbe antagonistic to dysentery bacilli. C. R. Acad. Sci. 165, 373–375.
- Fruciano, D.E. and Bourne, S. (2007) Phage as an antimicrobial agent: d’Herelle’s heretical theories and their role in the decline of phage prophylaxis in the West. Can. J. Infect. Dis. Med. Microbiol. 18(1), 19-26.
- Johnson, B. (2023) Microbiome-friendly phages join the campaign for better antimicrobials. Nat. Biotechnol. 41, 438–439.
- Venhorst, J. et al. (2022) Battling enteropathogenic Clostridia: phage therapy for Clostridioides difficile and Clostridium perfringens. Front. Microbiol. 13, 891790.
- Liu, H. et al. (2023) Therapeutic potential of bacteriophage endolysins for infections caused by Gram‑positive bacteria. J. Biomed. Sci. 30, 29.
- Gerstmans, H. et al. (2016) From endolysins to Artilysin®s: novel enzyme-based approaches to kill drug-resistant bacteria. Biochem. Soc. Trans. 44, 123–128.
- Bens, L. et al. (2023) Phage therapy for hidradenitis suppurativa: a unique challenge and opportunity for personalized treatment of a complex, inflammatory disease. Clin. Exp. Dermatol. DOI: 10.1093/ced/llad207
- Pirnay, J.P. (2020) Phage therapy in the year 2035. Front. Microbiol. 11, 1171.
Related Posts
Latest posts by Ken Doyle (see all)
- Will Artificial Intelligence (AI) Transform the Future of Life Science Research? - February 1, 2024
- RAF Inhibitors: Quantifying Drug-Target Occupancy at Active RAS-RAF Complexes in Live Cells - September 5, 2023
- Synthetic Biology: Minimal Cell, Maximal Opportunity - July 25, 2023
