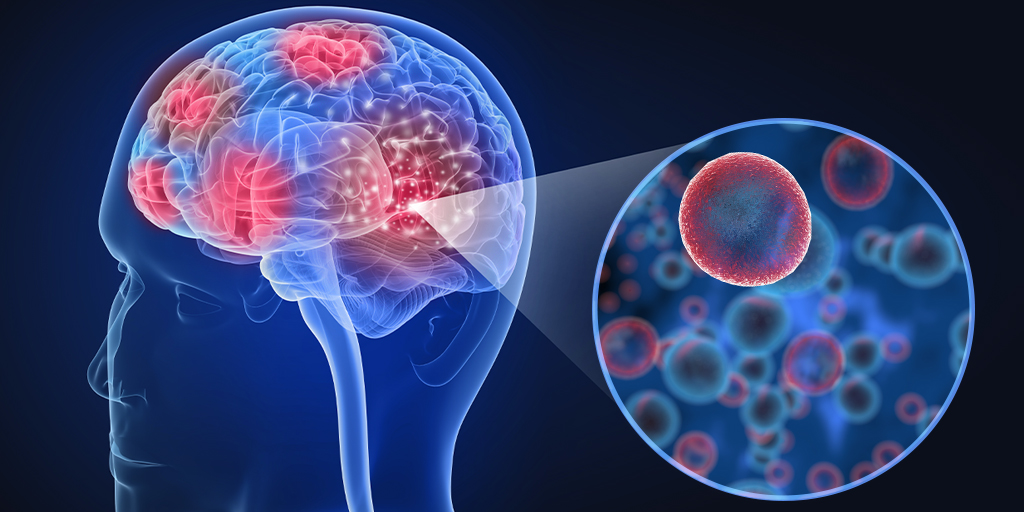
Alzheimer’s disease is a devastating, progressive degenerative brain condition that starts with mild dementia symptoms like memory issues and gradually worsens to the point where you can no longer communicate or care for yourself. For anyone with personal experience with it, Alzheimer’s looms like a specter over the natural process of aging.
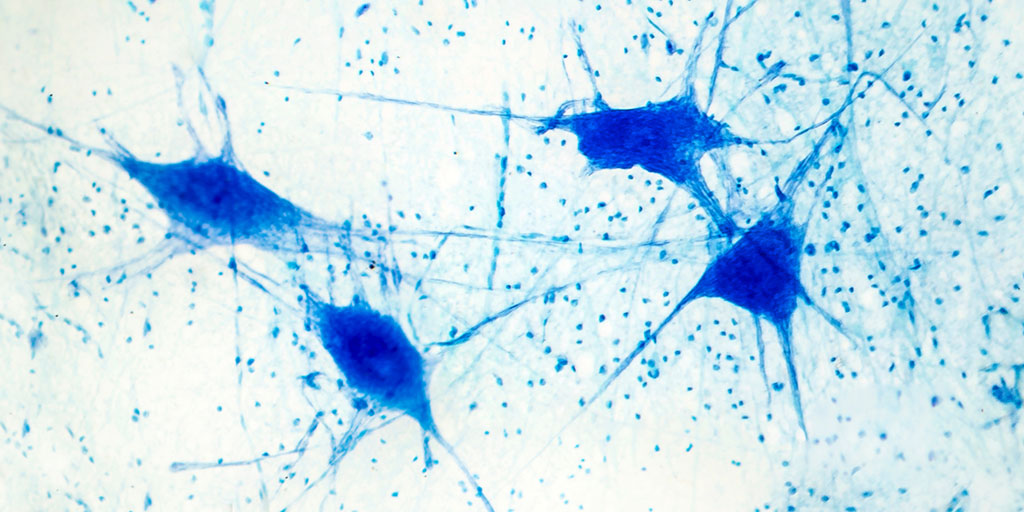
In the beginning phase of Alzheimer’s, abnormal plaques of the protein, amyloid-β, develop. These protein clumps can accumulate for decades with no detectable impact on cognitive ability or brain health. Eventually, a second protein, tau, begins to gather and form intercellular, fibrous, tangles. It is with the formation of these tau tangles that symptoms first appear. The combined presence of these extracellular plaques and intercellular tangles are the hallmarks of Alzheimer’s disease.
Continue reading “T Cells Newly Discovered Role in Alzheimer’s and Related Diseases Could Offer Another Therapeutic Approach”