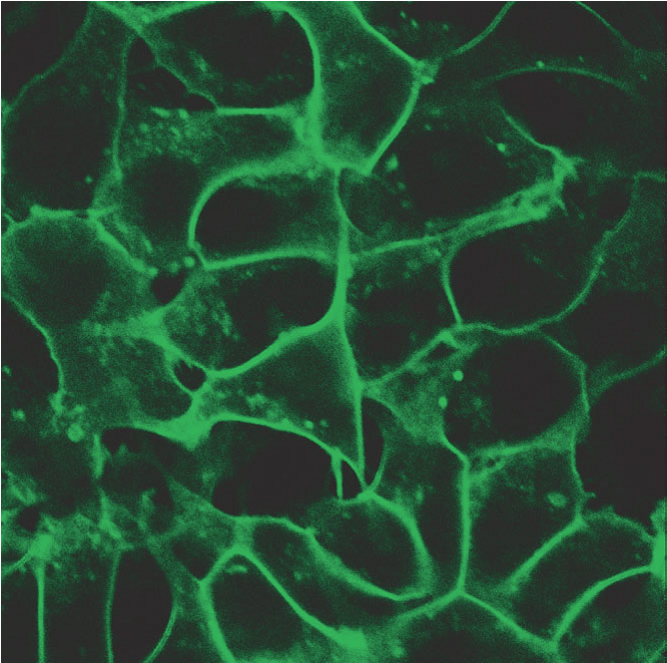
Cell signaling is a finely tuned process where both timing and spatial context play essential roles. Whether it’s a hormone triggering a cellular response or a drug modulating a pathway, these processes unfold in dynamic, spatially organized ways. To study them, researchers rely on chemigenetic biosensors—genetically encoded tools that light up in response to molecular activity. However, traditional biosensors are constrained by several limitations: poor photostability under prolonged imaging, limited spectral flexibility for multiplexing, and insufficient spatial resolution for studying signaling events at subcellular scales.
Continue reading “Seeing Signals in a New Light: Far-Red Chemigenetic Biosensors Illuminate Kinase Activity”