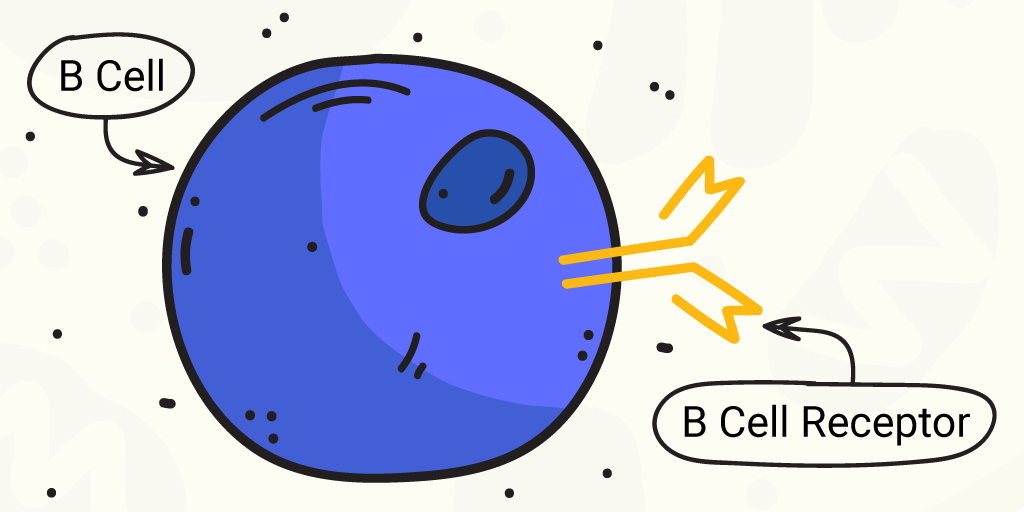
B cells are the immune cells that produce antibodies (immunoglobulins or Ig) to detect intruding pathogens. B cells produce a variety of classes of antibodies. Generally during an immune response to a pathogen, whether viral or bacterial, B cells produce immunoglobulins (Ig) IgM and IgD, and later in the response, IgG and IgA, that are specific to the intruding organism. These Igs capture and aid in neutralizing the pathogen.
Ig classes can be studied by sequencing the B cell receptor (BCR), which binds antigen specifically. BCRs are formed via irreversible gene segment rearrangements of variable, diversity and joining (VDJ) genes. Ig classes can be diversified through somatic hypermutation and class-switch recombination of these gene segments (1).
B cell receptors with high sequence similarity can be found in individuals exposed to the same antigen, demonstrating that antigen exposure can result in similar B cell clones and memory B cells between individuals, both adults and children (1).
However, B cell immune responses can differ between adults and children. For example, children use more B cell clones that form neutralizing antibodies to HIV-1. And children infected with SARS-CoV-2 generally have milder illness than infected adults. SARS-CoV-2-infected children have lower antibody titers to the virus and more IgG-specific response to SARS-CoV-2 spike protein than to the nucleocapsid protein (1). These differences can contribute to faster SARS-CoV-2 clearance and lower viral loads in children versus adults.
Investigating Antibody Response Over the Human Life Span
Yang et al. studied changes in antigen-specific B cell memory over the human life span and across tissues, by characterizing uniformity in immunoglobulin (Ig) heavy chain (IGH) sequences specific for 6 common pathogens as well as 2 viruses not encountered by the participants, Ebola virus and SARS-CoV-2, in pre-COVID-19 pandemic individuals.
Study specimens included 12 cord blood samples; blood samples from 51 children aged 1 to 3 years and 114 blood samples from healthy human adults aged 17 to 87 years. They also analyzed B cells from blood, lymph node and spleen samples from 8 deceased organ donors.
Need a reminder about antibody response and immunity? Check out this Promega Connections blog post.
Children in this study had been vaccinated to typical childhood pathogens including H. influenzae type B, Pneumococcal pneumoniae and tetanus toxoid on a typical vaccination schedule of 2, 4, 6 and 12 to 15 months, had influenza virus (flu) vaccination and were probably exposed to respiratory syncytial virus (RSV).
The authors note that the children were not vaccinated against N. meningitidis and that the childhood vaccination status of the adult participants was unknown.
Results
As might be expected, cord blood (collected from umbilical cords at birth) showed the least uniformity in comparison to reference Igs, consistent with limited fetal pathogen and vaccine exposure.
Uniformity in B cell clones for the noted pathogens were seen in children and adults, and were largely IgM and IgD, with limited class switching.
In adults, clones specific for H. influenza B, N. meningititis and RSV were generally IgM and IgD, with no class switching, while clones for Pneumococcal vaccine, tetanus toxoid and influenza virus were class switched.
Blood contains only a fraction of a person’s B cell repertoire; spleen, lymph nodes and the gut contain many B cells and are recognized as major sites of Ig somatic hypermutation and class switching. Noting the lack of class-switched clones for adults, the researchers looked at adult tissues (blood, mediastinal and mesenteric lymph nodes and spleen) to determine the frequency of class-switched Igs to H. influenza B, N. meningititis and RSV. They found uniformity of clones in lymph nodes and spleen, but not in blood, suggesting limited distribution of clones in adult circulation.
Furthermore, adult lymph nodes and blood from children showed greater uniformity of clones than seen when comparing adult and child blood, supporting a difference in distribution between adults and children.
An interesting additional finding was that prepandemic children had class-switched clones to SARS-CoV-2 and related variants, but not to Ebola virus, causing the authors to suggest that previous coronavirus exposure could form cross-reactive memory B cells.
What’s Next?
Yang et al. note that further study of cross-reactive memory B cells and their role in response to related pathogens is needed. Further understanding of the determinants of memory B cell is needed to better support vaccine production, both to SARS-CoV-2 variants and potentially other new or emerging pathogens.
Reference
- Yang, F. et al. (2021) Shared B cell memory to coronaviruses and other pathogens varies in human age groups and tissues. Science 372, 738–41.
Related Posts
Kari Kenefick
Latest posts by Kari Kenefick (see all)
- Fluorescent Ligands in Biological Research: Where We’ve Been, Where We’re Headed - June 27, 2024
- Cell-Based Target Engagement and Functional Assays for NLRP3 Inhibitor Profiling Help Identify Successes and Failures - January 25, 2024
- Illuminating the Brain with a New Bioluminescence Imaging Substrate - April 13, 2023
