HBO’s The Last of Us has successfully brought fungal pathogens to the forefront of the pandemic discourse, raising questions as to whether a fungus could really pose a significant threat to humans. While scientists agree that the fungus featured in the show, cordyceps, won’t be making the required inter-species jump any time soon, there is a fungal pathogen that has been taking root in hospitals across the U.S. which gives some cause for concern: Candida auris.
What is Candida auris?
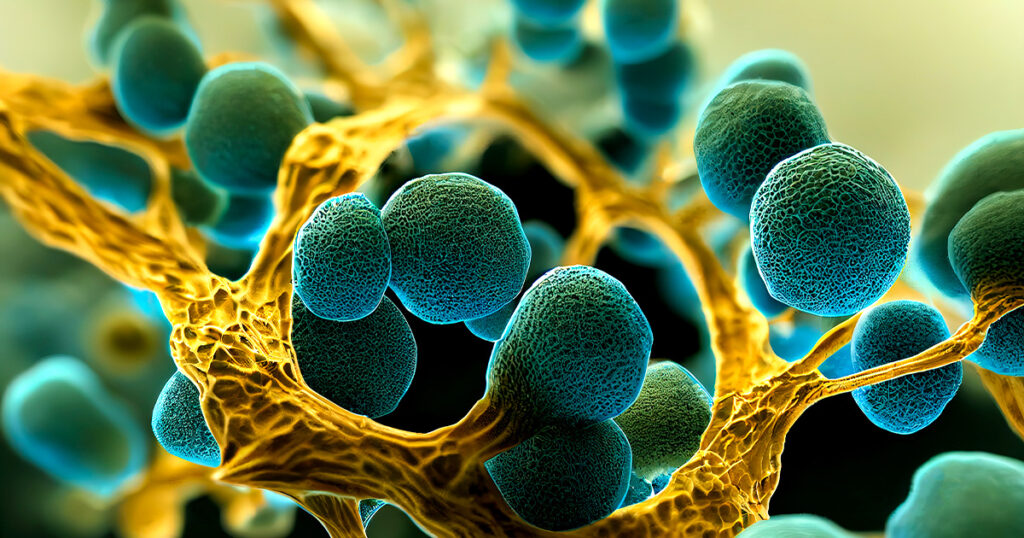
Candida auris is a yeast that tends to proliferate in healthcare settings, including hospitals and nursing homes, and is notorious for being remarkably resistant to antifungal medications. Since it was initially detected in the U.S. in 2016, the fungus has now appeared in half of U.S. states and is said to have spread widely during the COVID-19 pandemic, clinging to protective gear like gowns and gloves as well as invasive medical equipment like ventilators, catheters and feeding tubes3. According to the CDC, between 2016 and 2021 there were 3,270 clinical cases reported across the country, and 7,413 cases in which the fungus was present but did not cause active infection5. Though roughly half of all infected patients have died, it is not clear whether all of these deaths are due to the fungus alone or to comorbidities3.
How did Candida auris emerge?
In sequencing the Candida auris genome, scientists found at least four genetically distinct populations of the fungus that seem to have emerged simultaneously, independently and in separate regions around the globe1. Whether these strains all originated in one place or if each region experienced local emergence, the source of the pathogen is difficult to pinpoint due to variables like global trade and travel. But how did Candida auris become such a big problem, seemingly overnight?
Evidence so far has pointed to healthcare networks as a primary source of transmission, particularly long-term care facilities where patients are severely ill and immunocompromised1. Candida auris has been observed to be impervious to many disinfectants and persists on indoor surfaces like furniture, medical equipment, and clothing, as well as human skin. A lack of adequate prevention methods and poor control of the spread may have been contributing factors in the recent and significant increase in case counts. These problems would have grown worse during the pandemic, where COVID-19 was a priority and other pathogens took a back seat.
As to how the fungus came to be so resilient, some scientists have posited theories that implicate global environmental changes, large-scale human activity and rising temperatures. The extensive use of fungicide in farming and pharmaceutical manufacturing could result in the release of these chemicals into the environment through runoff or effluent, leading to lower fungal diversity and making room for drug-resistant strains of Candida to gain a foothold1. Though there are few fungi that can tolerate mammalian body heat, rising temperatures around the globe may also select for strains of fungus that can grow in warmer conditions4. While these theories would require further study to be considered seriously, they put forward interesting questions about the potential role of anthropogenic activity in the emergence and spread of new pathogens like this one.
Stopping the spread of Candida auris
While researchers toil away at the bench in search of a vaccine, the best strategies for confronting Candida auris as it stands are improved lab infrastructure and better detection methods2. The more efficiently a lab can deliver an accurate diagnosis after receiving a sample, the sooner measures can be taken to contain the fungus and limit exposure. More proactive screening processes for patients who are high-risk will also help healthcare facilities manage spread.
Additionally, testing wastewater can alert facilities to the presence of Candida auris quickly and efficiently. A wastewater detection kit like the GoTaq® Enviro Candida auris qPCR System from Promega, which includes the target FKS1 gene that codes for antimicrobial resistance in Candida, can help facilities and communities identify whether the fungus is circulating and take the steps necessary to contain it6.
Despite its rather alarming progression, intensive containment measures do appear to be effective in mitigating the spread of Candida auris. Further study of the origins of this fungus and how it acquired such robust resistance to antifungal treatments will better equip us to address any similar pathogens that may emerge down to the road.
To inquire about the GoTaq® Enviro Candida auris qPCR System, reach out to our team at applied@promega.com.
Learn more about applying wastewater surveillance to detect emerging pathogens.
References:
- Jackson, B.R., Chow, N., Forsberg, K., Litvintseva, A.P., Lockhart, S.R., Welsh, R., Vallabhaneni, S.; Chiller, T. On the Origins of a Species: What Might Explain the Rise of Candida auris? J. Fungi 2019, 5, 58. https://doi.org/10.3390/jof5030058
- Candida auris: How the US can stop the spread of the deadly fungal infection – Vox
- Candida Auris, a Deadly Fungus, Spread Rapidly During Pandemic, CDC Says – The New York Times (nytimes.com)
- Climate change could raise the risk of deadly fungal infections in humans (sciencenews.org)
- CDC: Deadly Candida auris fungus spreading quickly through health care sites : NPR
- Leach, L., Zhu, Y., Chaturvedi, S. Development and Validation of a Real-Time PCR Assay for Rapid Detection of Candida auris from Surveillance Samples. Journal of Clinical Microbiology, 2018, Vol. 56, No. 2. https://journals.asm.org/doi/10.1128/JCM.01223-17
Related Posts
Latest posts by AnnaKay Kruger (see all)
- Elephants May Call Each Other By Name - July 16, 2024
- Studying Episodic Memory through Food-Caching Behavior in Birds - April 16, 2024
- A Silent Killer: Tracking the Spread of Xylella fastidiosa - March 27, 2024
