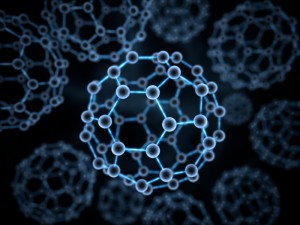
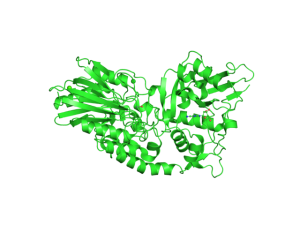
Silver nanoparticles (Ag-np) are commonly used in many consumer products, including cosmetics, textiles, electronics and medicine, largely due to their antimicrobial properties. More recently, Ag-np are being used to target and kill cancer cells. It has been known for years that silver nanoparticles (Ag-np) can induce cell death and DNA damage. Studies have also shown that Ag-np inhibit cell proliferation and induce apoptosis in cancer cells. However, cancer cells are able to fight back with DNA repair mechanisms such as non-homologous end joining repair (NHEJ). The NHEJ pathway requires the activation of DNA-dependent protein kinase catalytic subunit (DNA-PKcs), thus DNA-PKcs may protect against the Ag-np-induced DNA damage in cancer cells.
Could inhibition of DNA-PKcs increase the ability of Ag-np to kill cancer cells? In a 2017 study, Lim et al. wanted to test whether inhibition of DNA-PKcs can increase the cytotoxic effect of Ag-np in breast cancer and glioblastoma cell lines. To effectively determine cell viability in these cancer cell lines, the authors used the CellTiter-Glo® Luminescent Cell Viability Assay. The CellTiter-Glo® Assay determines the number of viable cells in culture based on quantitation of ATP, an indicator of metabolically active cells. A major advantage of this assay is its simplicity. This plate-based assay involves adding the single reagent (CellTiter-Glo® Reagent) directly to cells cultured in serum-supplemented medium. This generates a luminescent signal proportional to the amount of ATP present, which is detected using a luminometer. Cell washing, removal of medium and multiple pipetting steps are not required. Another advantage of the CellTiter-Glo® Assay is its high sensitivity. The system detects as few as 15 cells/well in a 384-well format in 10 minutes after adding reagent and mixing, making it ideal for automated high-throughput screening, cell proliferation and cytotoxicity assays.
The authors first confirmed that Ag-np treatment reduced proliferation and induced cell death/DNA damage in two breast cancer cell lines and two glioblastoma cell lines. The cytotoxic effect of Ag-np is specific to cancer cells, as minimal cytotoxicity was observed in non-cancerous human lung fibroblasts used as control. Next, they pre-treated the cancer cells with a DNA-PKcs inhibitor for 1 hour before adding Ag-np. Inhibition of DNA-PKcs increased Ag-np-mediated cell death in all four cancer cell lines. This suggests that DNA-PKcs may be protecting the cells from Ag-np cytotoxicity. The authors further showed that DNA-PKcs may repair Ag-np induced DNA damage by NHEJ and JNK1 pathways. In addition, DNA-PKcs may help recruit DNA repair machinery to damaged telomeres.
This study suggests that a combination of Ag-np treatment and DNA-PKcs inhibition may be a potential strategy to enhance the anticancer effect of Ag-np.
Reference: Hande M.P., et.al. (2017) DNA-dependent protein kinase modulates the anti-cancer properties of silver nanoparticles in human cancer cells. Mutat Res Gen Tox En. 824, 32
Like this:
Like Loading...