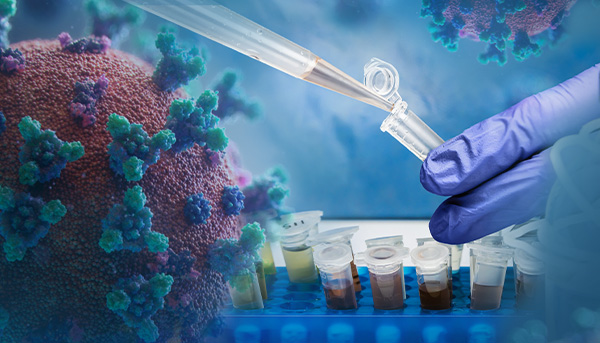
Before the COVID-19 global pandemic began, Dr. Xuping Xie, Assistant Professor of the University of Texas Medical Branch at Galveston, TX has been studying viruses, such as Dengue and Zika, for more than 10 years. Once the pandemic hit in early 2020, he was prepared to join the fight against the virus. “There was an urgent need to know: Is there a quicker way to develop therapeutics or antibodies to target SARS-CoV-2?” says Dr. Xie. “That’s why we immediately launched our SARS-CoV-2 project.”
His goal was to create an assay that could 1) screen for antiviral drugs and 2) quickly measure neutralizing antibody levels. The assay could be used to determine the immune status of previously infected individuals and to evaluate various vaccines under development. To achieve this, he wanted to create a reporter virus that is genetically stable and replicates similarly to the wild-type virus in cell culture.
Continue reading “A SARS-CoV-2 NanoLuc® Reporter Virus for Rapid Screening of Antivirals”