This blog was written in collaboration with Tian Yang, Associate Product Manager at Promega.
Cancer is often driven not only by genetic mutations, but by changes in how genes are turned on or off—epigenetic alterations. Two key players in this space are bromodomain and extra-terminal (BET) proteins and histone deacetylases (HDACs).
BET proteins help activate gene expression by recognizing acetylated lysines on histones, while HDACs remove these acetyl groups, repressing transcription. When these mechanisms become dysregulated, they can promote tumor growth or silence tumor suppressors.
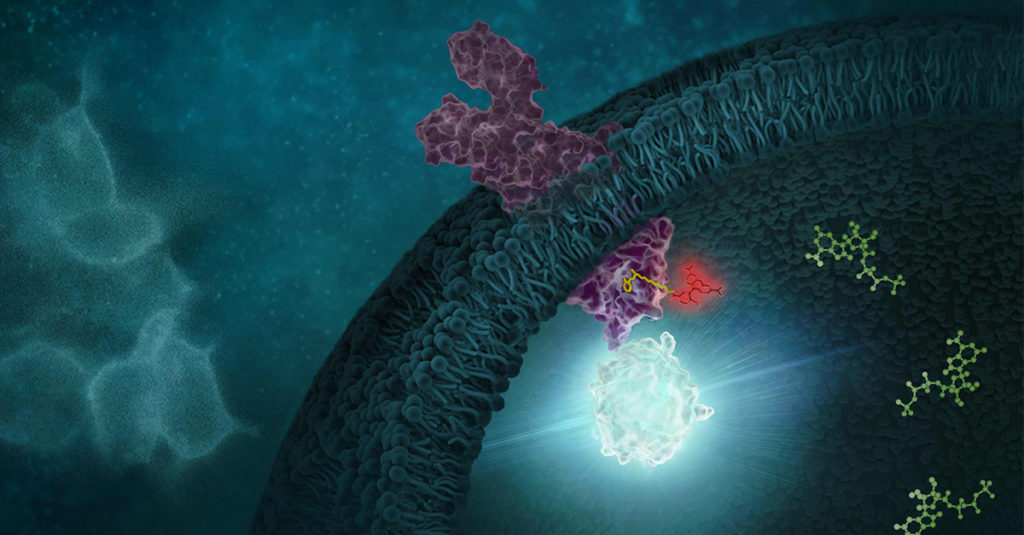
To counteract this dysregulation, researchers have developed inhibitors that target BET proteins and HDACs. While combinations of these drugs have shown synergy, using two separate compounds introduces challenges with dosing, toxicity and pharmacokinetics. Recent efforts have focused on designing multitarget inhibitors—single molecules that can simultaneously block BET and HDAC activity.
A Structure-Guided Approach to Dual BET/HDAC Inhibitors
In their paper, “Development of Potent Dual BET/HDAC Inhibitors via Pharmacophore Merging and Structure-Guided Optimization”, Bauer and colleagues aimed to design and optimize dual BET/HDAC inhibitors that would be effective in hard-to-treat cancers like pancreatic ductal adenocarcinoma (PDAC) and NUT midline carcinoma (NMC). Starting with known scaffolds from BET and class I HDAC inhibitors, they used pharmacophore merging and structure-guided design to create a new set of compounds capable of targeting both BRD4 (a key BET protein) and HDAC1/2 with high potency.
Their best-performing compounds showed submicromolar EC₅₀ values for both targets in cell-based NanoBRET™ assays, which measure inhibitor binding inside live cells. The NanoBRET™ assays provided precise, real-time readouts of compound engagement with BRD4 bromodomains and HDAC1/2, confirming that the designed inhibitors were active in a cellular context, not just in vitro.
Functionally, these dual inhibitors blocked histone H3 deacetylation, increased expression of HEXIM1 and p57 (known markers of BET inhibition), and downregulated MYC and TP63 in NMC cells. Importantly, the dual activity was linked to superior effects on cancer cell viability compared to individual BET or HDAC inhibitors. These results suggest that finely tuned dual inhibitors could be a powerful therapeutic strategy and a more manageable alternative to combination therapy.
Selective BET Inhibitors with Improved Tolerability in Inflammation Models
In their work, “Efficacy and Toxicity Analysis of Selective BET Bromodomain Inhibitors in Models of Inflammatory Liver Disease”, Doskey and colleagues focused on selectively inhibiting individual BET bromodomains to reduce inflammation without causing the toxicity seen in pan-BET inhibition. BET inhibitors have shown promise as anti-inflammatory agents, but clinical development has been hampered by side effects like thrombocytopenia and gastrointestinal damage. By targeting just the BRD4-D1 domain—or combining BRD4-D1 with a pan-D1 profile—the authors aimed to maintain efficacy while improving safety.
Their study tested a panel of orally bioavailable BET inhibitors in models of inflammatory liver disease. Using NanoBRET™ assays, they quantified how well each compound engaged its BET targets inside live cells. The assays revealed that compounds with BRD4-D1 or pan-D1 selectivity had effective intracellular engagement, although some had lower permeability.
In two mouse models—LPS-induced inflammation and acetaminophen-induced liver injury—the BRD4-D1 and pan-D1-biased inhibitors reduced pro-inflammatory chemokines like CXCL1 and CCL2 and limited liver tissue necrosis. Promisingly, these inhibitors also showed reduced thrombocytopenia in megakaryocyte colony-forming assays. However, some still caused goblet cell loss in the gut, indicating that BRD4 may still play a role in gastrointestinal toxicity.
The authors suggest that future refinements of BRD4-D1 inhibitors—with better pharmacokinetics and reduced off-target effects—could yield safer therapies for chronic inflammation and potentially cancer.
Conclusion
These two studies highlight the therapeutic potential of precisely targeted epigenetic inhibitors. Whether through dual-action compounds that tackle BET and HDAC activity at once, or domain-selective BET inhibitors designed to minimize side effects, the field continues to move toward smarter, safer small molecules. The NanoBRET™ Target Engagement Assays have been instrumental in confirming that these new compounds hit their targets in live cells, helping bridge the gap between molecular design and real-world biological effect.
Latest posts by Promega (see all)
- Compact Design, Big Impact: Tridek-One Therapeutics Leverages MyGlo® to Accelerate Discovery of Immunomodulating Treatments - October 22, 2025
- One Health in Action: Integrated Solutions for Animal Health Pathogens - October 14, 2025
- Measure Engagement to Target Proteins within Complexes: Why Context Matters - October 9, 2025
