One Milk Marketing Board campaign uses celebrities to promote its product by photographing them with milk moustaches. Glamour aside, selling cow’s milk is important to the livelihood of many farmers worldwide and generates a variety of well-appreciated products. What would pizza be without cheese? Summer without ice cream? Lunches without yogurt? Mashed potatoes without butter? Flammkuchen without crème fraiche? You can see where I am going with this. I live in America’s Dairyland where people commonly drink milk with meals. I think there is nothing better than a cold glass of milk with a rich chocolate cake. However, the Milk Marketing Board has missed a significant finding: milk fats can attenuate metastasis and some of the systemic effects of cancer and chemotherapy—at least in mice.
Sun et al. set out to discover if feeding bovine milk butter fat to mice would have any effect on tumor formation, metastasis and the side effects of paclitaxel, a chemotherapy treatment for breast cancer. The authors cited previous studies that had found anti-cancer compounds in milk fatty acids and the reduced risk of mammary tumors for mice fed an anhydrous milk fat (AMF) diet. Therefore, they took 48 female Balb/c mice, a common laboratory strain, and fed them either a control diet with soybean oil as the fat or a milk fat diet, which substituted AMF for the oil, keeping the percentage fat the same for both diets. After two weeks, the mice were injected with either breast or colon cancer cells derived from Balb/c cultured cell lines. When the tumors reached 0.5cm, 12 of the tumor-bearing mice were injected with paclitaxel. See the table below for the matrix of conditions.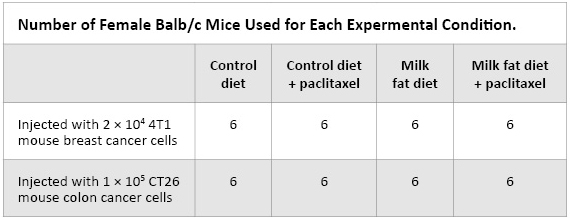
The mice fed the milk fat diet delayed forming tumors by two (4TI) or three (CT26) days compared to those on the control diet. Interestingly, for the mice on the milk fat diet alone and injected with 4TI breast cancer cells, the effect on the tumor size was nearly the same as the control diet + paclitaxel. The rate of tumor growth was unaffected by diet differences but once paclitaxel was injected, the mice on the milk fat diet + paclitaxel showed a greater decrease in tumor diameter compared to those on control + paclitaxel.
These effects on tumor formation and size carried over to analysis of metastases. Both cancer cell lines selected are known to metastasize to liver and lung. Once the tumors in the control-diet mice reached 1cm (28 days for mice injected with CT26 cells and 35 days for mice injected with 4TI cells), all the mice were euthanized, and the liver and lungs removed for assessing organ weight and counting of metastatic tumors. The control mice had the most metastatic tumors, the milk fat diet mice had fewer, paclitaxel treatment reduced the number of tumors in both control and milk fat-fed mice but the combination of milk fat diet and paclitaxel yielded the fewest tumor spots on the lungs and liver. This reduction was also reflected in the weights of the organs, the control mice lungs and liver weighing more than any of the other treatment groups and the milk fat + paclitaxel-treated mice weighing the least.
Sun et al. also examined tumor angiogenesis, counting the number of blood vessels found in sections of tumors and staining sections with Anti-CD31 antibody; the protein CD31 is expressed on the endothelial cells lining blood vessels and a good marker for angiogenesis in tumors. When counting the vessels stained by the antibody, the density was lower for milk fat diet and paclitaxel-treated mice compared to the control. The median distance between the stain vessels was reduced for mice on the milk fat diet and mice on control diet treated with paclitaxel. However, as with the other assessments, milk fat diet + paclitaxel treatment together were most effective in reducing angiogenesis.
The AMF fed to the mice is effective at reducing tumor size, vascularization and metastases formation in lungs and liver but were there other effects in mice? 4TI breast cancer cell line was used because once it metastasizes, it causes wasting in mouse model, similar to what is seen in advanced cancer in humans. Mice on the control diet and control diet + paclitaxel lost more than 10% of their body weight with noticeable loses in gastrocnemius muscle and ovarian fat deposits compared to mice on the same diet without tumors or paclitaxel treatment. Not surprisingly, tumor-bearing and nontumor-bearing mice fed the milk fat diet weighed more than those on the control diet with increased weights for both muscle and adipose tissues. Thus, tumor-bearing mice were better able to keep on weight and reduce the loss of muscle when fed milk fat.
Not only the cancer but the treatment can cause systemic effects. Paclitaxel affects more than just the tumor but also damages the intestinal villi, exacerbating the problem of weight loss. However, the authors found mice with tumors feed milk fat with or without paclitaxel kept the weight. To examine the effects of diet and paclitaxel treatment, mice without tumors were feed either control or milk fat diet for two weeks, paclitaxel administered and then euthanized after 1 week. The villi in the jejuna of the intestine were examined in healthy mice and regardless of the diet, the villi were found intact. However, for mice without tumors on the control diet and treated with paclitaxel, villi were were broken and flat. The mice given milk fat + paclitaxel had jejuna with intact villi. The length of the villi were measured and found that mice treated with paclitaxel had reduced average villi length but the milk fat-fed mice lost only 28% compared to 52% those on control diet. These differences in results carried through when assessing γ-glutamyl transpeptidase (γ-GGT), a marker for epithelium in the small intestine, and apoptotic bodies that precede the damaged villi. These data demonstrated milk fat diet partially ammelorates the damage to the intestine caused by paclitaxel.
Another problem with both cancer and chemotherapy is suppression of blood cell synthesis, ultimately affecting the ability of the body to fight infections. In mice with 4TI tumors on the control diet, red blood cell (RBC) and white blood cell (WBC) counts decreased 23% and 28%, respectively, compared to healthy mice on the control diet. For the mice with tumors on control diet + paclitaxel, the blood cell count reductions went even further, resulting in a 8.6% decrease in spleen weight. However, mice on milk fat diet + paclitaxel only had minor RBC and WBC decreases (11% or less) with a small decrease in spleen weight. For mice with 4TI tumors on the milk fat diet, the WBC decreased 9% with a small increase in RBC numbers and equivalent spleen weights to healthy mice on control diet. In these measures, milk fat has a protective effect for mice with 4TI tumors with the greatest difference measured between mice on control diet + paclitaxel and those on milk fat diet + paclitaxel.
This study was intriguing because the last thing I expected was to find that milk fat, albeit in a concentrated form, would offer such a protective benefit for mice injected with breast or colon cancer cells. The antitumor activity added on top of paclitaxel was significant, and AMF demonstrated additional benefits (maintaining body weight and blood cell counts) that likely assist the chemotherapy in fighting cancer. So while we are unlikely to see campaigns showing mice with milk mustaches anytime soon, I think the Milk Marketing Board has some new opportunities for the future.
Reference
Sun X, Zhang J, Gupta R, Macgibbon AK, Kuhn-Sherlock B, & Krissansen GW (2011). Dairy milk fat augments paclitaxel therapy to suppress tumour metastasis in mice, and protects against the side-effects of chemotherapy. Clinical & experimental metastasis PMID: 21739249
Sara Klink
Latest posts by Sara Klink (see all)
- A One-Two Punch to Knock Out HIV - September 28, 2021
- Toxicity Studies in Organoid Models: Developing an Alternative to Animal Testing - June 10, 2021
- Herd Immunity: What the Flock Are You Talking About? - May 10, 2021

Great post! I wonder if part of the reason for milk’s antitumor activity has to do with lactose: cancer cells do not metabolize lactose as easily as glucose. In fact, cancer cells preferentially use glucose via glycolysis (Warburg effect). Perhaps the milk sugar and fat are having an effect on the cancer cells by making it hard for them to gain adequate nutrition?