Neurodegenerative disorders represent a significant and growing concern in the realm of public health, particularly as global populations age. Among these, Parkinson’s disease (PD) stands out due to its increasing prevalence and profound impact on individuals. Characterized by the progressive degeneration of motor functions, PD is not just a health challenge but also poses substantial socio-economic burdens. While the etiology of Parkinson’s disease is far from simple, current research efforts elucidating its causes, mechanisms, and potential treatments illustrate the critical nature of this neurodegenerative disorder in today’s healthcare landscape.
In the clinic, Parkinson’s disease is often diagnosed as either sporadic or familial. Familial PD has a clear genetic basis, typically passed down through families, while sporadic PD, comprising about 90% of cases, occurs in individuals without a known family history of the disease. The exact cause of sporadic PD is not fully understood but is believed to be due to a combination of genetic predispositions and environmental factors. In contrast, the factors involved in familial PD are more thoroughly understood, offering insights into the molecular mechanisms underlying PD pathogenesis.
Polymorphisms and Parkinson’s Disease Susceptibility
Among the factors increasing the risk of PD onset includes certain genetic polymorphisms or variations in the DNA sequence that commonly occur within a population. These genetic variations can influence an individual’s susceptibility to PD by affecting critical biological processes including protein degradation, mitochondrial function, and dopamine metabolism, which are crucial in PD pathogenesis. Notably, mutations in genes such as SNCA, which encodes the alpha-synuclein protein involved in Lewy body formation, and LRRK2, a gene implicated in cellular autophagy and mitochondrial dynamics, have been associated with an increased risk in developing PD. Recently, a study published by Cuttler et al. in the Journal of Neural Transmission revealed that mutations in neurexin 2α (NRXN2α), an important gene for synaptic function, are another possible contributor to Parkinson’s disease. These associations underscore the importance of genetics in PD and enable the development of potential targeted therapies.
A Novel Synaptic Gene Polymorphism
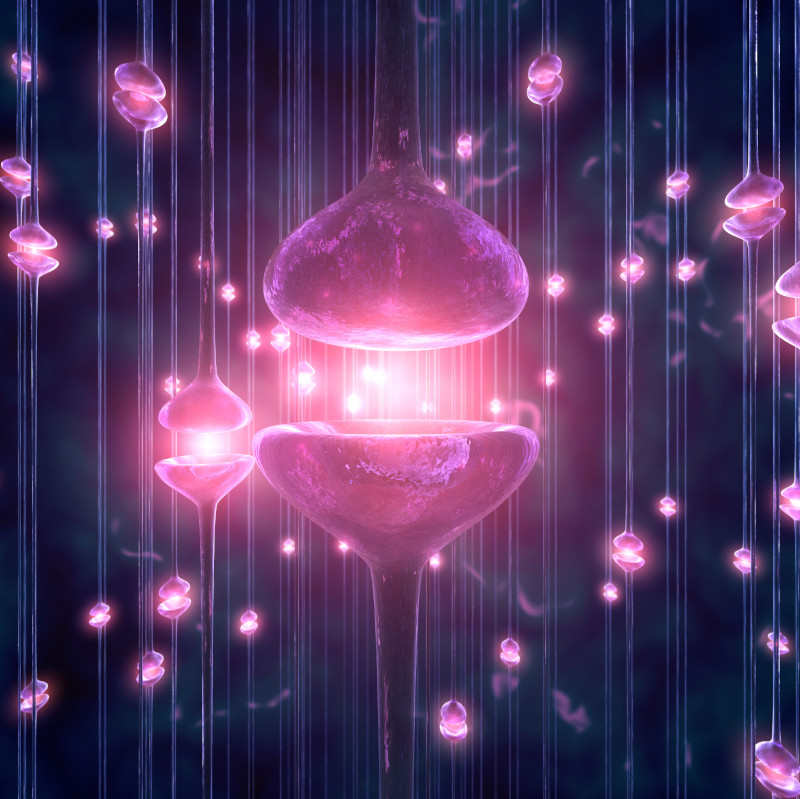
To better understand how a gene variation in NRXN2α impacts PD onset, Cuttler et al. transfected SH-SY5Y cells, a neuroblastoma cell line, with a wild-type or mutated NRXN2α variant plasmid and evaluated its impact on cell health in vitro. A prior study from this research group identified one gene variant, p.G849D in neurexin 2α, as a potential candidate for Parkinson’s disease (Sebate et al, 2021). This variant has an autosomal dominant mode of inheritance, meaning one copy of the mutated gene (from one parent) is enough to cause the disorder. Neurexins are a family of presynaptic cell adhesion proteins that interact with various postsynaptic partners to regulate synapse maintenance and function. When there are disruptions in synaptic function, it could contribute to impaired dopaminergic transmission, a hallmark of PD, or exacerbate existing neuroinflammatory and neurodegenerative processes.
Through their experiments, Cuttler et al. observed that cells overexpressing mutant NRXN2α plasmid had decreased cell viability and metabolic activity, quantified using the ApoTox-Glo™ Triplex Assay and an MTT assay, respectively. The ApoTox-Glo™ Triplex Assay measures cell viability, cytotoxicity, and apoptosis from the same sample well. This is an important tool because it allows the mechanism of cell death to be determined without using additional sample. Among these samples there were no reported differences in cytotoxicity or apoptosis measures, further suggesting that mutant NRXN2α overexpression does not induce cytotoxicity or apoptosis.
This study also explores how the mutant NRXN2α plasmid affects mitochondrial health by measuring changes in mitochondrial membrane potential (MMP), which decreases during cell death as mitochondrial permeability increases. Here, the overexpression of mutant NRXN2α in cells had negative impacts on mitochondrial function, diminishing MMP. Lowered MMP across the mitochondria results in reduced ATP generation, affecting energy available in synapses and their normal functioning.
Additionally, the impact of mutant NRXN2α overexpression on the production of reactive oxygen species (ROS) was investigated by monitoring changes in hydrogen peroxide (H2O2) levels, an indicator for oxidative stress, which was quantified using the ROS-Glo™ H2O2 Assay. Briefly, an H2O2 substrate reacts directly with H2O2, creating a luciferin precursor. The addition of the ROS-Glo™ Detection Solution converts the luciferin precursor to luciferin, resulting in luminescence that is proportional to H2O2 in the sample well. The results from this assay suggest that SH-SY5Y cells overexpressing mutant NRXN2α exhibit significantly higher levels of ROS compared to cells exposed to the wild-type plasmid. ROS, which is normally produced by the mitochondria and is necessary for cell homeostasis, can cause oxidative stress and even cell death when its production is dysregulated.
Conclusions
In summary, this study evaluates the impact of mutant NRXN2α overexpression on cell health, mitochondrial health, and ROS production and implicates that the p.G849D gene variation in NRXN2α is associated with mitochondrial dysfunction. Importantly, the data evaluating mitochondrial function suggests that overexpression of mutant NRXN2α adversely impacts MMP and ROS production, leading to decreased ATP production and increased oxidative stress. Both energy depletion and/or increased oxidative damage can contribute to local disturbances in calcium homeostasis and degeneration of synapses, further contributing to neurodegenerative processes. The authors suggest that the NRXN2α mutation may initiate a potential toxic feedback loop where mitochondrial dysfunction or an imbalance in ROS leads to escalated oxidative stress, which in turn adversely affects mitochondrial functionality. While this work implicates a synaptic protein variant associated with PD in mitochondrial dysfunction, additional studies using PD cellular models or animal models are needed to further verify these findings. As research progresses, insights into how these polymorphisms influence the onset and progression of PD may lead to more personalized medicine approaches in treatment, emphasizing the critical role of genetics in the fight against PD.
References
Sebate, B., Cuttler, K., Cloete, R., Britz, M., Christoffels, A., Williams, M., Carr, J., & Bardien, S. (2021). Prioritization of candidate genes for a South African family with Parkinson’s disease using in-silico tools. PLoS One, 16(3), e0249324. https://doi.org/10.1371/journal.pone.0249324
Cuttler, K., de Swardt, D., Engelbrecht, L., Kriel, J., Cloete, R., & Bardien, S. (2022). Neurexin 2 p.G849D variant, implicated in Parkinson’s disease, increases reactive oxygen species, and reduces cell viability and mitochondrial membrane potential in SH-SY5Y cells. Journal of neural transmission, 129(12), 1435-1446. https://doi.org/10.1007/s00702-022-02548-8
