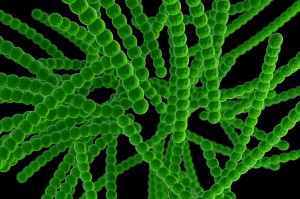
Salmonella. Streptococcus. Shigella. The most well-known bacteria are those that cause disease. Our relationship with them is one of combat. With good reason, we look for ways to avoid encountering them and to eliminate them when we do meet.
But not all bacteria are bad for us. Of course we have known for years that we are colonized by harmless bacteria, but recently, studies on the human microbiome have revealed many surprising things about these bacterial tenants. Studies are showing that the teeming multitudes of organisms living in and on the human body are not just harmless bystanders, but complex, interrelated communities that can have profound effects on our health.
Three studies published in Science in 2018 add more to the growing body of microbiome surprises, showing that certain gut bacteria are not only good for us, but may even be required for the effectiveness of some anti-cancer immunotherapies.
In his book “I Contain Multitudes”, author Ed Yong recounts many fascinating stories coming out of microbiome research, including connections between previously unknown gut bacteria and the control of inflammation, obesity and other metabolic diseases. This research has resulted in a paradigm-shift in how we view bacterial colonization. Yong states:
This is what medicine looks like when you understand that microbes are not the enemies of animals, but the foundations upon which our kingdom is built. Say goodbye to dated and dangerous war metaphors, in which we are soldiers hell-bent on eradicating germs at whatever cost. Say hello to a gentler and more nuanced gardening metaphor. Yes, we still have to pull out the weeds, but we also seed and feed the species that bind the soil, freshen the air and please the eye.
Recent discoveries suggest that in the future, deliberate and individualized cultivation of the microbiome to introduce desirable bacterial species could be part of a very personalized approach to the treatment of disease.
The authors of the Science papers studied the gut microbiome composition of responders and non-responders to immunotherapy in melanoma (Gopalakrishnan et al, Matson et al), non-small cell lung, renal and uroepithelial cancers (Routy et al). They found that the presence of bacteria of the genus Faecalibacterium, Bifidobacterium or Akkermansia in the gut of patients treated with immune checkpoint inhibitors was associated with improved outcomes.
Routy et al found that antibiotic use immediately before PD-1 immunotherapy was associated with decreased treatment effectiveness. Analysis of the gut organisms from responders and non-responders showed that colonization with the bacterium Akkermancia muciniphilia was associated with positive outcomes. In follow up experiments, they showed that colonization of mice with Akkermancia alone was sufficient to cause a positive response to PD-1 mAb treatment, and addition of Akkermancia to the guts of mice colonized with non-responder bacteria restored sensitivity to treatment.
All three studies showed that bacteria play a critical role in response to immunotherapy, but the positive effect was associated with different groups of bacteria in each case. The exact reasons why these bacteria enhance responsiveness to immunotherapy remains to be identified. However, the research raises the intriguing possibility of manipulating gut bacteria during treatment to increase the likelihood of success. Knowledge that intestinal bacteria influence treatment effectiveness could also help avoid treatments, such as antibiotics, that may negatively affect the microbiome composition before immunotherapy.
Faecalibacterium. Bifidobacterium. Akkermansia. We are only beginning to know and to name the bacteria that actively contribute to our good. What we know is still eclipsed by what we do not know about these organisms. Learning about them is becoming an exciting journey of discovery about ourselves and redefining how we view our “tenants”.
Papers
- Pespective: Jobin, C. (2018) Precision medicine using microbiota. Science 05 Jan: 359(6371), 32-34. DOI: 10.1126/science.aar2946
- Routy, B., et al (2018) Gut microbiome influences efficacy of PD-1–based immunotherapy against epithelial tumors. Science 359(6371), 91-97. DOI: 10.1126/science.aan3706
- Gopalakrishnan, V., et al (2018) Gut microbiome modulates response to anti–PD-1 immunotherapy in melanoma patients. Science 05 Jan: 359(6371), 97-103. DOI: 10.1126/science.aan4236
- Matson, V., et al (2018) The commensal microbiome is associated with anti–PD-1 efficacy in metastatic melanoma patients. Science 05 Jan: 359(6371), 104-108. DOI: 10.1126/science.aao3290
Isobel Maciver
Latest posts by Isobel Maciver (see all)
- 3D Cell Culture Models: Challenges for Cell-Based Assays - August 12, 2021
- Measuring Changing Metabolism in Cancer Cells - May 4, 2021
- A Quick Method for A Tailing PCR Products - July 8, 2019
