
In 2012, a 6-year-old girl named Emily Whitehead was battling acute lymphoblastic leukemia (ALL), one of the most common cancers in children. Her cancer was stubborn. After 16 months of chemotherapy, the cancer still would not go into remission. There was nothing else the doctors could do, and she was sent home. She was expected to survive only a few more months. Her parents would not give up and enrolled her into a clinical trial of a new immunotherapy treatment called chimeric antigen receptor (CAR) T cell therapy. She was the first pediatric patient in the program.
Doctors took T cells from Emily’s blood and reprogrammed them in a lab. They essentially sent her T cells to boot camp where they are trained to find cancer cells and destroy them. The reprogrammed T cells were then injected back into her body. A week into treatment, she started getting a fever, the first sign that the treatment was working and her reprogrammed T cells were fighting the cancer. But soon, she got very sick. All of the indicators suggested that she had cytokine release syndrome (CRS)—also known as the cytokine storm. This happens when cytokines are released in response to an infection but the process cannot be turned off. The cytokines continue to attract immune cells to the infection site, causing damage to the patient’s own cells and eventually resulting in acute respiratory distress syndrome (ARDS). (Learn more about the cytokine storm in this blog.)
Emily was soon on a ventilator. Tests showed that she had extremely high levels of one particular cytokine: interleukin-6 (IL-6). Desperate to keep her alive, her doctors gave her a known drug that specifically targets IL-6. The results were dramatic. After one single dose, her fever subsided within hours, and she was taken off the ventilator. On May 2nd, 2012, she woke up from an induced coma—it was her 7th birthday. Her doctors said they have never seen a patient that sick get better that quickly.
The drug that saved her life was tocilizumab.
IL-6 and Tocilizumab
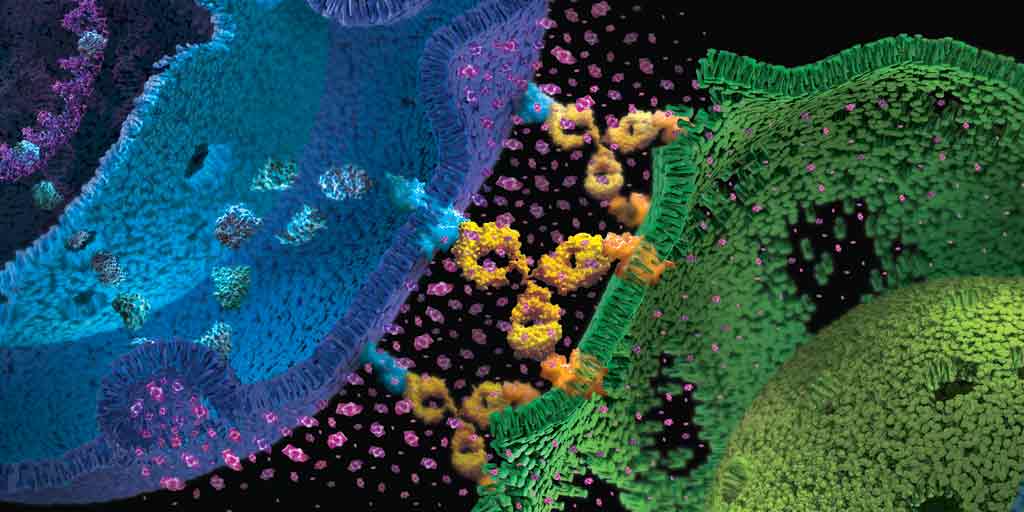
IL-6 is a multifunctional cytokine produced by endothelial cells and various immune cells (e.g., T cells, macrophages, and monocytes). It plays a central role in inflammation, such as promoting T cell activity and B cell differentiation, and regulating the acute phase response following tissue injury. IL-6 works by binding to its receptor, IL-6R, which could be free-floating in the cell or attached to the cell membrane. Once IL-6 and IL-6R are bound together, the complex can then attach to another membrane protein (gp130) and trigger a variety of intracellular signals.
Because of the critical role of IL-6 in the immune response, it became an enticing target for drug development. One such drug is tocilizumab. Tocilizumab is an engineered protein (scientifically speaking, it’s a humanized monoclonal antibody) that specifically binds IL-6R. When IL-6R binds to tocilizumab, it can no longer bind to IL-6, therefore inhibiting interaction with gp130 and all downstream inflammatory signaling. Tocilizumab was first approved in 2010 for the treatment of rheumatoid arthritis, an autoimmune disorder that causes swelling and pain in the joints.
From CAR T to COVID-19
Only three weeks after starting the CAR T cell treatment, Emily’s cancer was in remission. In the following years, as CAR T cell therapy became more widespread, researchers found that roughly 70% of patients develop CRS, and that tocilizumab is a highly effective treatment. In 2017, the FDA approved the use of tocilizumab for the treatment of patients with CAR T cell-induced CRS.
Fast forward to 2020: We are amidst a global pandemic due to the rapid spread of a deadly flu-like disease called COVID-19. A subset of the most severe COVID-19 patients develop CRS, and again, IL-6 levels are high in these patients. Doctors began testing the use of tocilizumab on these patients, and in many cases, it saved their lives. In China, a small clinical trial with 21 patients showed that, within the first day of receiving tocilizumab, the fever subsided in all patients. Oxygen intake was reduced in 75% of patients.
Just this week, the preliminary results of a clinical trial in France with 129 COVID-19 patients (64 received tocilizumab, 65 did not) was announced. In the tocilizumab treatment group, both the number of deaths and the need for later ventilator support were significantly reduced.
These preliminary results are encouraging, and more studies are underway to fully understand the effect of tocilizumab on COVID-19 patients—and potential side effects. Because tocilizumab works by suppressing the IL-6 immune response, it may increase the risk of secondary infection. Other known side effects include pancreatitis and gastrointestinal perforations, which can be dangerous for those with pre-existing conditions.
IL-6 Targeted Therapy
The versatile use of tocilizumab from treating rheumatoid arthritis, to CAR T-cell-induced CRS, to COVID-19, suggests that new uses for existing IL-6 drugs will continue to be discovered. For example, if tocilizumab is successful in treating CRS in COVID-19 patients, it is possible that IL-6 targeted therapies can be used to help patients infected with other viruses, such as influenza or Ebola.
Does your research project involve detecting cytokines? Learn about the Lumit™ assays for detecting cytokines in cell culture samples.
Tocilizumab isn’t the only drug targeting IL-6. In the last 10 years, other IL-6 inhibitors have been developed and tested for treating a variety of conditions. In 2014, a drug called siltuximab that binds IL-6 directly, was approved for treating Castleman disease (a rare disorder that causes enlarged lymph nodes). Sarilumab, an antibody that binds IL-6R (similar to tocilizumab), was approved for treating rheumatoid arthritis in 2017. A number of ongoing studies are testing IL-6 targeted therapies on other conditions, including eye diseases, depression, schizophrenia and heart attacks. It’s clear that we’ve only scratched the surface of the therapeutic potential of IL-6 inhibition.
Tomorrow is Emily’s 15th birthday, in which she will be celebrating 8 years of being cancer free. She survived not only because of the CAR T cell therapy, but also thanks to tocilizumab, which kept her alive as her immune cells wiped out the cancer in her body. There is no doubt that tocilizumab and other IL-6 inhibitors will continue to save the lives of those suffering from cancer, COVID-19 and beyond.
Learn more about our bioassays that can be used to characterize and develop novel antibody-based therapeutics targeting cytokines such as IL-6.
References
Zhang, C. et al. (2020) The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. [Epub ahead of print]
Moore, J. B. and June, C. H. (2020) Cytokine release syndrome in severe COVID-19. Science [Epub ahead of print]
Choy, E.H. et al. (2020) Translating IL-6 biology into effective treatments. Nat Rev Rheumatol. [Epub ahead of print]
Anti IL-6 For Coronavirus Patients: Does It Work, or Not?
Emily Whitehead: A Young Girl Beats Cancer with Immunotherapy
Emily Whitehead’s Story: CAR T Cell Therapy for Acute Lymphoblastic Leukemia
Related Posts
Latest posts by Johanna Lee (see all)
- How Avian Influenza Crosses Species - February 22, 2024
- Macrophages: The Unsung Heroes of Immune Response and Biologic Drug Development - December 28, 2023
- Treating Solid Tumors: Combining CAR-T Cell Therapy with Probiotics - October 31, 2023
