When it comes to blocking the spread of viral pathogens that cause human disease, epidemiologists—people who study disease outbreaks—like to talk about herd immunity. But what do they mean when discussing the herd and their immunity? Today, I will tackle this subject but with a side jaunt: I am going to co-opt the word “herd” and replace it with “flock” thus making chickens the center of attention rather than cattle for this analogy about immunity in a population. (Disclaimer: I am utterly biased toward chickens and enjoy talking about my flock of 24 hens and pullets).
Who is the Herd Flock They Keep Talking About?
By using a collective term for a number of individuals such as “herd” or “flock”, epidemiologists and public health experts are referring to a population or community. Doing some investigation, I learned herd immunity was a term first used in 1917 and referred to…cows. That makes sense, right? When we talk about groups of cattle, the term used is “herd”. Turns out there was an infection that caused spontaneous miscarriages in cattle and became epidemic in American herds. Farmers managed this threat by destroying or selling the infected cows. However, a livestock veterinarian had a different view, describing this pathogen as “…a fire, which, if new fuel is not constantly added, soon dies down. Herd immunity is developed, therefore, by retaining the immune cows, raising the calves, and avoiding the introduction of foreign cattle” (1). Essentially, this veterinarian was noting that keeping the infected cows who had immunity against the contagion meant the herd were less likely to be reinfected and, thus, put an end to the epidemic.
The term herd immunity was again used in a 1923 article when a bacteriologist was describing experiments he conducted, creating epidemics in mice, noting that without adding susceptible mice, the epidemic ended. From this report, the term moved from animals into human medicine when a professor of pathology drew parallels between what was reported about the mice epidemics and his observations of diptheria epidemics that affected schoolboys in the UK (1,2). Once in the public health consciousness, this analogy between immunity in cattle herds and that of human populations kept being used and reused.
However, as more vaccines became available in the mid 20th century, public health experts began asking what percentage of the herd, flock or population needed to be vaccinated to control or eliminate a disease-causing pathogen? This is where much of the discussion comes in and the crux of the matter regardless if we are talking about the current SARS-CoV-2 outbreak or any other virus. The population under discussion can be a small as an apartment complex or town and as large as the entire global community. But those concerned with infectious disease outbreaks need to know: How big does the immunity firewall need to be to keep the targeted virus from spreading? That is, what percentage of the community needs to have immunity to block a virus from finding susceptible individuals where it could replicate and spread? For epidemiologists and others involved in communicating about public health, analogies to herds, flocks or firewalls are ways to describe why immunity is important for the population and in your community.
How Does Herd Flock Immunity Work?
Flock immunity is like playing bumper cars at the amusement park. If one car is carrying a viral cargo around the rink, but eight of the nine cars it bumps into are immune, delivery of the infectious package to a susceptible target is difficult. The greater number of individuals are immune, the more difficult it becomes for the virus to find someone it could infect. Conversely, if a person is infected, having a greater number of immune people around will block the virus from finding a susceptible host.
However, the level of immunity in a flock needs to be above a threshold to be able to douse the infection and prevent it from spreading. Vaccination is the best method get the needed immunity levels in a population. While exposure to a virus and recovery from infection will leave an individual with immunity, the public health goal is to avoid infections that result in disease, suffering and death. Vaccines prime an individual’s immune system to recognize an invader and increase the collective immunity in a population, thus becoming a preventative measure in the case of epidemics or pandemics. By creating a wall of numerous immune people around those individuals who are susceptible to infection and unable to be vaccinated, flock immunity blocks viral spread and protects the vulnerable.
What are the Factors Involved in Herd Flock Immunity?
The first consideration is some people are unable to be vaccinated. For those that are too young, pregnant or immunocompromised, vaccination is not an option for them. As a result, that means we cannot achieve 100% immunity and need to be concerned about protecting these individuals from the circulating virus. Vaccines are still the best tool for making a greater percentage of the population immune without disease. The higher that immunity number can reach, the greater likelihood an infection would be doused before it can take hold in a vulnerable population and spread.
Another consideration is how infectious a virus is. One that lives on surfaces for a few hours and can be easily managed with hand washing is less infectious than one that hangs around the air in respiratory droplets. The case studies shared throughout the SARS-CoV-2 pandemic have highlighted how spending time in enclosed rooms with an infected person not only results in several cases of COVID-19 for those that shared the same space, but also caused secondary and tertiary infections when those that were infected brought the virus back with them, exposing their family and neighbors as well. All the talk about viral variants has highlighted how much more infectious these strains of SARS-CoV-2 are compared the original circulating strain. To calm the spread of the contagion and prevent further mutations, high levels of immunity are needed for the flock. With the original virus, a threshold of 60–70% may have worked, but the newer variants health experts are discussing 80% or greater levels of immunity.
Why Should I Care About the Herd Flock?
If we want everyone to return to the kind of public life we saw in 2019 rather than 2020, flock immunity is the way to achieve that. In the beginning, we used nonpharmaceutical interventions to manage disease spread: Wear a mask, social distance and wash your hands. Or as the scientists and clinicians of the web site Dear Pandemic say: Stay SMART
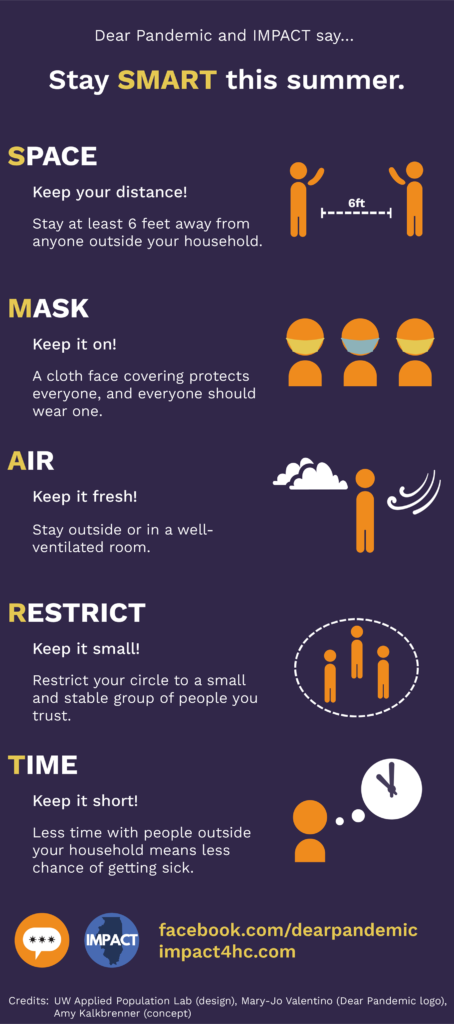
Continuing these behaviors can help mitigate disease spread especially with public health concerns about the more transmissible variants becoming the dominant circulating viral strains. Of note, the nearly nonexistent flu season demonstrates how effective these measures can be . However, vaccination can get everyone closer to those longed-for gatherings and events. With more vaccines being distributed and administered, we have the opportunity to increase the immunity of our population and protect those who cannot get a vaccine or face serious illness when infected.
Herd Flock immunity helps protect your friend undergoing cancer treatment, your elderly grandmother, your neighbor’s newborn, your sister who has an organ transplant, your cousin who has an autoimmune disease, your pregnant niece and your uncle who has diabetes. Keeping the nasty viruses away from the people you care about is important. Vaccination will block a virus seeking to infect those around you and build up immunity in the community.
Summary
Herd Flock immunity refers to the number of immune individuals in a population that can prevent infected people from spreading disease to the community. With enough of the population immune to an infectious disease, that percentage, the immunity threshold, can stop viral infection in its tracks. This immunity protects those with compromised immune systems and prevents disease and death within a community. Polio and smallpox have been essentially eliminated using vaccination and the population immunity strategy. Vaccines work by keeping the susceptible population low and decreasing the spread of SARS-CoV-2 or any other infectious disease to those we care about.
Population Immunity References
- Jones, D. and Helmreich, S. (2020) A history of herd immunity. Lancet 396, 810–811.
- Malein, F. (2020) Herd Immunity – what’s in a name? British Society for the History of Medicine web site. Accessed May 10, 2021.
Sara Klink
Latest posts by Sara Klink (see all)
- A One-Two Punch to Knock Out HIV - September 28, 2021
- Toxicity Studies in Organoid Models: Developing an Alternative to Animal Testing - June 10, 2021
- Herd Immunity: What the Flock Are You Talking About? - May 10, 2021
