The pandemic caused by SARS-CoV-2 has brought the world to its knees. There have been many deaths, many persons with lingering disease (long COVID) and the inability to vaccinate everyone quickly, for starters. SARS-CoV-2 has not only been a tricky adversary in terms of treatment options to save lives, it’s also been a wily opponent to researchers studying the virus.
Contributing to the existing studies, with their review of the role of inflammasomes in COVID-19, Vora et al. recently published “Inflammasome activation at the crux of severe COVID-19” in Nature Reviews Immunology. In this paper they detail evidence of inflammasome activation and its role in SARS-CoV-2 infections.
Contributions of Those Lost in the SARS-CoV-2 Pandemic
I’d like to take a moment to note the uniquely awful nature of the virus at the center of this blog and the paper it reviews. Many of the papers we blog about describe research involving cell lines, mice or another animal model. The closest most reports get to human research subjects is the use of human cells lines. In the Vora et al. report, serum and tissue samples are from actual human patients, some that survived and many that did not survive COVID-19. It’s not lost on us, Dear Reader, the contributions of those that suffered and died due to SARS-CoV-2 infection. Many persons with severe or fatal COVID-19 have made a significant contribution to our understanding of this virus and its treatment options. We owe them, as well as the researchers that have studied SARS-CoV-2, our sincerest gratitude.
Why the Interest in Inflammasomes?
For detailed information on inflammasomes you can read Ken’s blog, here. You will find background information there and on our inflammasome web page.
In their paper, Vora et al. provide evidence of inflammasome activation, both direct and indirect, in COVID-19. The authors note:
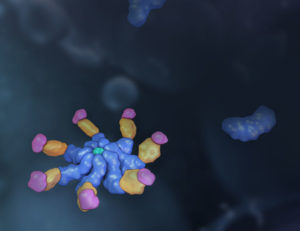
“Key to inflammation and innate immunity, inflammasomes are large, micrometrescale multiprotein cytosolic complexes that assemble in response to pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) and trigger proinflammatory cytokine release as well as pyroptosis, a proinflammatory lytic cell death.”
Evidence of inflammasome activation includes:
- Damage to cells resulting in lactate dehydrogenase (LDH) release and a rise in serum LDH. Increased serum LDH is seen as the strongest predictor of severe disease.
- Elevated serum chemokines and other factors of inflammation such as C-reactive protein, IL-6 and TNFalpha. Additionally, IL-18 secretion, a “highly predictive biomarker of death”, is seen in patients with severe disease and is a result of inflammasome formation.
- IL-1beta-associated cytokines are implicated, but IL-1beta itself has short half-life and thus is difficult to measure and rely on as an indicator of severe COVID-19 in patient samples. However, IL-1RA (receptor antagonist) is frequently used as a surrogate for IL-1beta, and elevated IL-1RA is consistently seen with severe COVID-19. In addition, post-mortem histological sections of lung tissue have stained positive for IL-1beta compared to control sections.
- Inflammasome specks were identified in monocytes from infected patient monocytes.
- Plasma from COVID-19 patients was found to contain lipopolysaccharide (LPS) from bacterial cell walls, as well as bacterial DNA. Secondary bacterial infection is commonly seen in virus-infected lungs, indicated by the presence of LPS. LPS activates both NLRP3 and AIM2 inflammasomes.
What About Cytokine Storm?
We’ve heard about the severity of cytokine storm in COVID-19 patients. How is that connected to inflammasome activation? Activation of inflammasomes can become a massive feedback loop, initiated by viral, bacterial or other cellular insults, and then triggering subsequent additional inflammasome activation. IL-1beta attachment to the IL-1 receptor (IL-1R) causes a nuclear factor-kappa beta (NFkB) response to increase transcription of pro-IL-1beta in cells that are recruited to infected lungs. This results in further monocyte and macrophage recruitment with additional cytokine release, perpetuating the feedback loop. The end result can be a massive influx of monocytes and neutrophils associated with acute respiratory distress syndrome (ARDS). This cellular invasion is a contributor to the severe lung damage seen in some COVID-19 patients.
The human immune system does include controls to prevent massive over-reaction. But a response as overzealous as what has occurred in cases of COVID-19 cytokine storm, particularly in diabetic, lung- or heart-disease patients or obese persons with already hyperactivated immune systems, can prove deadly. The immune system brakes in these cases, simply cannot stop the train that is inflammation.
Blood Clots Associated with Inflammasomes
Some COVID-19 infections have also been characterized by blood clots and thrombosis. Coagulation events are known to occur with other viruses, including H1N1 influenza and SARS-CoV. The coagulation is accompanied by increased amounts of plasma clotting factors such as von Willebrand factor, D-dimer and factor VIII. It is known that GSDMD (pyroptotic executor protein gasdermin D), activated by inflammasomes, as well as pyroptosis (cell lysis due to inflammation), can trigger intense coagulation in the absence of cytokines. (Inflammatory caspases cleave GSDMD into fragments, then the amino-terminal fragment binds to lipids, oligomerizes and inserts a pore into the cell membrane. These pores direct the release of IL-1b and IL-18.)
As an example of coagulation linked to inflammasomes, the authors note a mouse model of endotoxemia where inflammasome signaling by caspase 1 or caspase 11 led to massive fibrin deposits.
The Remedies
SARS-CoV-2 infection has led to the need for creative, quick thinking about existing therapies that can block or slow inflammasome activation. Some existing therapies successful in blocking inflammasomes have shown success with SARS-CoV-2 as well.
Anakinra: This drug is a recombinant human IL-1RA, and has been used in small trials where it showed mixed results on both mortality and the need for ventilation. The authors note, however, that this drug was studied in patients with mild disease, and suggest that those with more severe disease might be a better fit for the drug.
Multiple phase II clinical trials are testing direct NLRP3 inhibition in patients with either mild or severe COVID-19. Inhibiting NLRP3 reduced cytokine release and lung inflammation in influenza A virus infection in animal models. A few of the drugs being tested for NLRP3 inhibition are:
- MCC950, an NLRP3 inhibitor, decreased caspase 1 activation and IL-1beta release in human monocytes infected with SARS- CoV-2. The diabetes drug glyburide, an NLRP3 inhibitor, reduced IL-6 release by SARS-CoV-2-infected human monocytes.
- Colchicine: The microtubule depolymerizer colchine, an indirect NLRP3 inhibitor known to block inflammasome formation, is being tested. Colchicine has been used for many years and is a well-tolerated drug. In a small trial, colchicine showed the ability to reduce patient dependence on oxygenation and hospitalization.
- Metformin: This diabetes drug is an indirect inhibitor of NLRP3 via mTOR, and in trials it significantly reduced mortality in COVID19 patients with type 2 diabetes. In mouse studies, metformin inhibited NLRP3 activation and inflammation in SARS-CoV-2-infected lungs.
GSDMD inhibition is an attractive target in inflammasome inhibition after SARS-CoV-2 infection, as pore formation caused by the amino-terminal GSDMD fragment, occurs prior to DAMP and IL-1B release. GSDMD inhibitors include:
- Disulfiram (DSF): This drug, approved by the US Food and Drug Administration (FDA) for the treatment of alcohol addiction, blocks GSDMD pore formation, protecting against LPS-induced sepsis and cytokine release.
- Dimethyl fumarate (DMF): This FDA-approved drug used for multiple sclerosis, was recently shown to inhibit GSDMD. A review of several patients with multiple sclerosis who were under DMF therapy, showed their SARS-CoV-2 infections to be self-limiting with no additional treatment.
Next Steps
The authors note that inflammasome and IL-1B activation or release has been shown to be protective against many pathogens in the acute phase of infection. However, continued stimulation and release of these proteins has deleterious effects in chronic disease. It is yet to be determined whether inflammasome signaling can be protective in SARS-CoV-2 infection.
They further note that timing of treatment in SARS-CoV-2 infection will be very important in order to achieve benefits while blocking the negative consequences of inflammasome activation in COVID-19.
Reference
Vora, S.M., Lieberman, J., Wu, H. (2021) Inflammasome activation at the crux of severe COVID-19. Nat. Rev. Immunol. doi: 10.1038/s41577-021-00588-x. Epub ahead of print.
Kari Kenefick
Latest posts by Kari Kenefick (see all)
- Cell-Based Target Engagement and Functional Assays for NLRP3 Inhibitor Profiling Help Identify Successes and Failures - January 25, 2024
- Illuminating the Brain with a New Bioluminescence Imaging Substrate - April 13, 2023
- Made Just for You: Promega Custom Reagents - October 28, 2022
