Ebola virus has received a lot of press in the last year due to the extended epidemic outbreak in Africa. Ebola is part of the family of Filioviruses (filamentous virus) and causes hemorrhagic fever that leads to internal bleeding and loss of bodily fluids. As the epidemic in Africa has illustrated so starkly, once the virus infects a large enough population, the human suffering it causes is devastating to individuals and communities. Because no treatment other than palliative fluid support is available to those infected by Ebola virus, virologists have focused attention on potential therapeutics and vaccines. The vaccine strategies now in clinical trials are based on a single Ebola virus glycoprotein, GP, and involve a DNA-based vaccine or innoculation with an Ebola protein expressed from a viral vector. How effective and safe this approach may be for protection from Ebola virus infection is currently under investigation.
Based on the history of effective vaccines, Marzi et al. was interested in testing a whole-virus vaccine for Ebola (EBOV). A whole-virus-based vaccine like smallpox or measles uses an attenuated or inactivated virus. The advantage of this method is that all the proteins as well as the nucleic acid are available for immunological reaction, offering broader-based protection than a single protein. In the recently published Science report from Marzi et al., a replication-incompetent Ebola virus was used as the basis for a whole-virus vaccine that was tested for its efficacy in nonhuman primates.
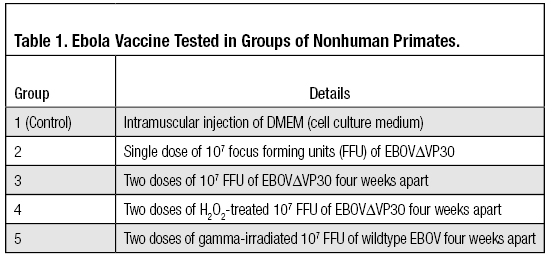
Previous work using the replication-incompetent EBOVΔVP30 (lacks viral protein 30 [VP30]) showed the virus was not pathogenic in rodents, and rodents innoculated with EBOVΔVP30 were protected from infection by Ebola virus. With possible safety concerns over EBOVΔVP30 further mutating and recovering replication competency, Marzi et al. decided to inactivate the virus using hydrogen peroxide and use that to generate a possible vaccine. This inactivation strategy has been used successfully to eliminate a virus’s ability to replicate while preserving its antigenicity. The virus was also exposed to gamma radiation, a method known to inactivate Ebola virus to examine the ability for this irradiated virus to be used as a vaccine. With these considerations, researchers had five groups of cynomolgus macaques innoculated as shown in Table 1. Groups 1–3 and 5 had four animals in each group and group 4 had two animals.
Whole-Virus Ebola Vaccine Protects Macques from EBOV Infection
Four weeks after immunization, all five groups of macaques, none of which showed any adverse effects to any of the vaccines tested, were challenged with 1,000 FFU (a lethal dose) of the Kikwit strain of EBOV. Groups 1 and 5 succumbed to EBOV infection while groups 2, 3 and 4 survived. Viral titers were tested in all animals, and groups 1 and 5 had high titers of EBOV while groups 3 and 4 had none. For macaques in group 2, one individual showed elevated levels of virus that cleared by day 9, while a second primate had a fever during the course of the testing. These results suggested that the single injection was not as effective at preventing EBOV infection but still allowed the nonhuman primates to survive a lethal dose of EBOV. The double injection of EBOVΔVP30 with or without H2O2 inactivation effectively protected the macaques from EBOV infection, while the gamma irradiated wildtype EBOV did not.
Whole-Virus Ebola Vaccine Evokes a Strong Immunity
The immune responses of the macaques were tested two and four weeks after the last vaccination using a GP-specific enzyme-linked immunosorbent assay (ELISA). This is the standard test used to assess the protective ability of an EBOV vaccine. The highest antibody titer came from group 3, while group 4 had a strong but lower response than group 3. Group 2 had a measurable IgG titer to GP, but neither group 1 nor 5 showed any antibody titer at all.
The authors also assessed the levels of two other viral proteins, viral matrix protein (VP40) and nucleoprotein (NP), using the macaque serum in protein-specific ELISAs. Groups 3 and 4 showed the highest titers of antibodies against VP40 and NP, while group 2 had lower levels of antibodies to VP40 and NP. In contrast to the GP-specific ELISA results, the gamma-irradiated wildtype EBOV-vaccinated animals (group 5) had antibodies react against VP40 and NP. The antibody titers were higher in animals that were protected from a lethal dose of EBOV, but researchers did not determine the significance of the levels of antibodies to VP40 and NP.
To further assess the antibody response, neutralizing antibody levels were tested using a plaque reduction neutralization (PRNT) assay. This assay measures the serum dilution that reduces the titer of vesicular stomatitis virus (VSV) expressing EBOV GP by ≥ 50% (PRNT50). For the macaques vaccinated twice with EBOVΔVP30 (group 3), PRNT50 was 1:20–1:40 while group 2 and 4 had lower PRNT50 titers of ~1:10. Groups 1 and 5 had no neutralizing titers. The titers in groups 2, 3 and 4 compared favorably with other PRNT50 values measured in other EBOV vaccinations studies.
Marzi et al. also tested cellular immunity in the vaccinated macaques by examining the number of mononuclear cells producing interferon gamma (IFNγ). Similar to the antibody-based assays, animals from groups 2 and 3 had the greatest number of IFNγ- producing cells. Group 4 animals had fewer IFNγ-producing cells but still had more than groups 1 and 5.
Conclusion
The results of a whole-virus EBOV vaccine whether replication-incompetent or H2O2-treated replication-incompetent EBOVΔVP30 was used, showed safe and effective protection for nonhuman primates. In addition, a single or double dose of the vaccine was sufficient to survive challenge by a lethal dose of wildtype Ebola virus. This offers significant advantages over other EBOV vaccines that require several injections for protection from infection. A whole-virus vaccine also offers more epitopes for a potential immune response, resulting in a more effective protection from Ebola virus infection than those vaccines based on a single viral protein currently in clinical testing.
Reference
Marzi, A., Hill-Batorski, L., Feldmann, F., Shupert, W.L., Neumann, G., Feldmann, H. and Kawaoka, Y. (2015) An Ebola whole-virus vaccine is protective in nonhuman primates Science.
Sara Klink
Latest posts by Sara Klink (see all)
- A One-Two Punch to Knock Out HIV - September 28, 2021
- Toxicity Studies in Organoid Models: Developing an Alternative to Animal Testing - June 10, 2021
- Herd Immunity: What the Flock Are You Talking About? - May 10, 2021
