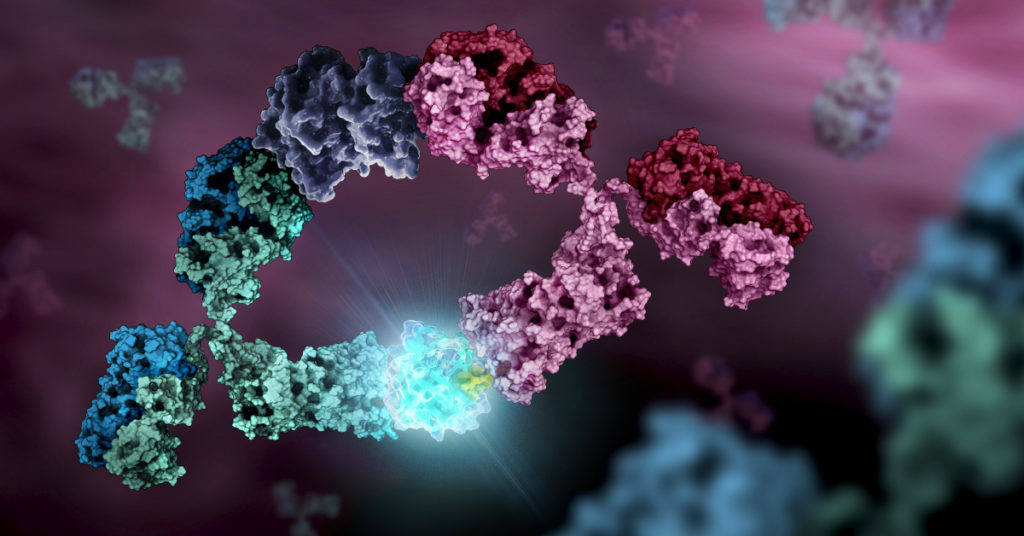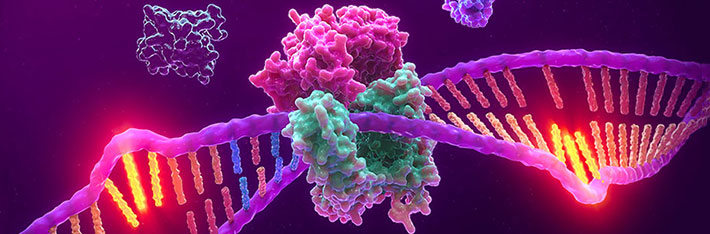
Chimeric Antigen Recepter (CAR)-T cell therapy is a personalized immunotherapy that harnesses the patient’s own immune system to combat cancer. It is done by engineering the patient’s T cells to specifically target and attack cancer cells in their body, and it has shown great success in treating various blood cancers such as leukemia.
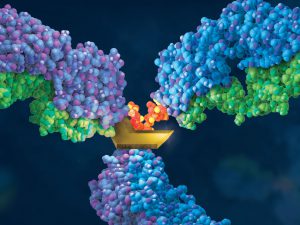
Treating solid tumors with CAR-T cells, however, has proved much more challenging. This is mainly because solid tumors contain a heterogeneous population of cells, expressing a variety of antigens—many of which are also expressed in healthy cells. Therefore, T cells targeting solid tumors could potentially attack healthy tissue, resulting in serious side effects. In addition, solid tumors create a hostile microenvironment that is difficult for CAR-T cells to infiltrate.
Continue reading “Treating Solid Tumors: Combining CAR-T Cell Therapy with Probiotics”